Managing CSF Leak After Pituitary Surgery – Advanced Reconstruction Strategies
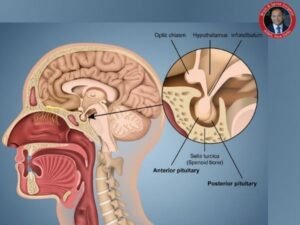
Topics Table of Contents Using sophisticated endoscopic procedures, pituitary surgery is a highly specialised treatment carried out through the nose. Even though pituitary surgery is