Topics
Table of Contents
Head Injury – Decompressive Craniectomy

Head injury is a major cause of morbidity and mortality worldwide, with traumatic brain injury (TBI) being a leading contributor to disability. Decompressive craniectomy (DC) is one of the most important life-saving surgical procedures for severe TBI, especially when persistent intracranial hypertension is present. The indications, methods, results, and debates around DC in the treatment of brain trauma are covered in this article.
Watch Full Video Playlist: Cadaveric Workshop – Brachial Plexus Surgery and Beyond
The cause of severe brain damage
Both primary and secondary damage processes are brought on by traumatic brain injury. Primary injuries, which include contusions, cuts, diffuse axonal damage, and haemorrhages, happen at the moment of impact. Over time, secondary damage develops as a result of processes such inflammation, excitotoxicity, cerebral oedema, and ischaemia. Poor outcomes are significantly predicted by elevated intracranial pressure (ICP) brought on by brain oedema. In order to prevent secondary brain injury, decompressive craniectomy aims to lower intracranial pressure and avoid cerebral herniation.
What is Decompressive Craniectomy?
Brain surgery that involves removing a part of the skull is called a decompressive craniectomy. Following an injury, the brain may enlarge, which can increase pressure inside the skull and result in more harm.

Swelling is the body’s normal healing reaction to damage. However, because the skull presses on the brain and limits the swelling, brain swelling can be harmful.
The danger of serious brain injury can be decreased and possibly saved by removing a part of the skull.
Decompressive Craniectomy – Quick Information

- Damage to the brain can result in harmful pressure that affects the brain, inhibits blood flow, and raises blood pressure.
- Brain swelling can occasionally result in lethal injuries.
- In order to lower brain pressure, a decompressive craniectomy involves removing a portion of the skull.
- Even after a decompressive craniectomy, a significant number of patients still pass away from brain oedema.
Why would you require one?
A decompressive craniectomy is most frequently performed for the following reasons:
- Traumatic Brain Injury (TBI): An injury to the brain caused by physical force is known as traumatic brain injury (TBI). Any event that causes a severe blow to the head may cause it. Brain swelling with a TBI is typically instantaneous.
- Stroke: Swelling of the brain can result from certain strokes. This swelling raises blood pressure, which increases the risk of more strokes.
When the brain expands and other methods of lowering pressure fail, doctors may think about doing a decompressive craniectomy.
Decompressive Craniectomy Indications
Patients with severe TBI who experience refractory intracranial hypertension in spite of receiving the best medical care may benefit from a decompressive craniectomy. Among the primary indicators are:
- Malignant cerebral edema: Caused by subsequent brain injuries, infarction, or trauma.
- ICP > 20–25 mmHg despite medical treatment (hyperosmolar therapy, sedation, CSF draining, controlled ventilation) is known as refractory intracranial hypertension.
- Lesions that occupy space include large bruises, haematomas, or infarcts that cause midline shifts and the mass effect.
- Clinical indicators of an impending or existing cerebral herniation include uncal or central herniation symptoms.
The process of decompressive craniectomy
- To relieve pressure on the brain, a decompressive craniectomy may involve the removal of a portion of the skull.
- The part of the skull that is putting pressure on the brain is removed by the surgeon during the procedure. Usually, the injury is covered by this region of the skull.
- Because the surgery is done under general anaesthesia, the patient will be unconscious, not aware of the process, and will not remember it.
- A cut to the scalp is the first step of a craniectomy. The skull is exposed when the surgeon removes the skin and tissue beneath it.
- Since the skull is a hard bone, the doctor will cut into it with a bone saw and a drill.
- The surgeon will stop any bleeding after removing the bone and then stitch the wound up.
- The bone removed from the skull during surgery is often kept in a freezer. The bone might be replaced if the patient heals.
Types of Decompressive Craniectomy
There are two distinct circumstances in which a decompressive craniectomy can be carried out.
- This study defines prophylactic decompression, also known as primary decompressive craniectomy (P-DC), as any surgical decompression procedure carried out on patients undergoing surgery primarily for the evacuation of any kind of intradural lesion, with or without the removal of brain tissue. Preventing anticipated postoperative increases in ICP (Intracranial Pressure) is the goal of prophylactic craniectomy, not controlling refractory ICP. The surgeon’s decision in these surgeries is typically based on intraoperative surgical observations (brain edema, a “tight” brain, or trouble moving the bone flap), a CT scan, or both. Typically, the surgeon’s decision is made independently of ICP.
- Therapeutic decompression, also known as secondary decompressive craniectomy (S-DC), is a surgery used on patients whose high Intracranial Pressure is not responding to medical treatment and who are under continuous ICP monitoring. When first- or second-line therapeutic methods have failed to control ICP, some centers turn to this therapeutic option. Patients who had an initial surgical surgery to remove a space-occupying lesion and later experienced delayed substantial unilateral or bilateral brain swelling were also included in the S-DC category. The goal of surgical decompression is to manage high ICP, even if these individuals may have had prior surgery.
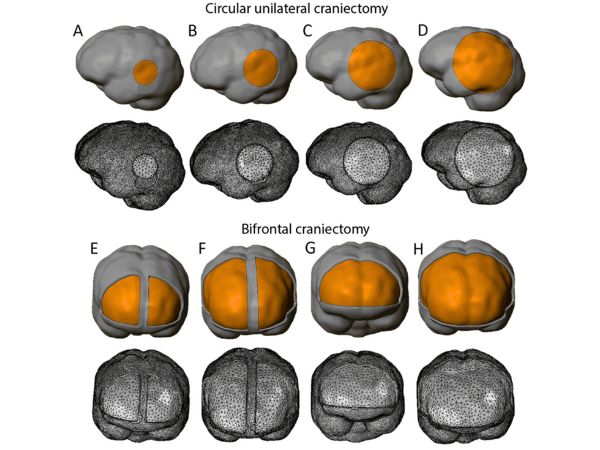
Decompressive craniectomy comes in two primary varieties in surgical approaches:

- Decompressive Craniectomy of the Bifrontal Area:
- Recommended for bilateral pathology and widespread cerebral edema.
- In order to make room for the enlarged brain, a huge bifrontal bone flap that extended from the supraorbital ridge to the coronal suture was removed.
- Unilateral (Hemicraniectomy) Decompressive Craniectomy:
- Usually carried out on patients who have unilateral lesions like severe contusions or big hemisphere infarcts.
- In order to allow for brain enlargement, bone flaps are removed from the temporal area to the parietal and frontal regions.
Usually, decompressive craniectomy is the last option.
Since brain surgery can be risky, especially for patients who have had a brain injury, medical professionals initially attempt nonsurgical treatments. These therapies could consist of:
- Oxygen therapy
- Medicines to reduce swelling
- Reducing body temperature
In order to lower the pressure, a doctor may occasionally attempt a less invasive procedure known as a ventriculostomy, which drains the cerebrospinal fluid.
What is the average duration of a stay in the hospital?

After surgery, the majority of patients will remain in the hospital for a few weeks. Recovery following the surgery and injuries may take months or even years. Following a decompressive craniectomy, a patient will need to be closely watched for any new indications of cerebral edema, and any infection symptoms will require immediate antibiotic therapy.
People can recover as much of their brain function as feasible with extensive rehabilitation. Exercise therapy, physical therapy, and speech therapy may fall under this category.
A surgeon will replace the missing part of the skull after the patient has fully recovered from the procedure and the initial damage. After the swelling has subsided, this treatment, known as a cranioplasty, provides the brain with additional protection.
The surgeon may use the original bone if it is healthy and hasn’t developed harmful bacteria. If not, titanium or synthetic bone may be used in its place.
Rehabilitation
Decompressive craniectomy patients are already in critical condition as a result of a stroke or brain injury. The time of their recovery is therefore largely determined by the injuries that initially needed surgery.
The majority of patients will stay in the critical care unit (ICU).
After surgery, some patients will be unconscious for several days or weeks. Some might even be vegetative or in a coma.
It is crucial to protect the brain from additional harm after a craniectomy. For weeks to months, the person must typically wear a helmet that has been specially fitted for them.
After Surgery Care
Postoperative care consists of:
- ICP monitoring is a continuous evaluation that helps avoid rebound swelling.
- Providing the best possible oxygenation and perfusion through haemodynamic and respiratory support.
- Complications include infection, hydrocephalus, CSF leakage, and syndrome of the trephined.
- Early Rehabilitation: Neurorehabilitation is started to enhance functional results.
Issues
The following are possible side effects of a decompressive craniectomy:
- Development of haemorrhages (either subdural or epidural collections)
- The need for ventriculoperitoneal shunting due to hydrocephalus
- Infections like wound dehiscence or meningitis
- Neurological decline brought on by the absence of bone surrounding the brain is known as syndrome of the trephined.
- Post-traumatic epilepsy and seizures.
Rate of Complications and Potential Concerns
Although decompressive craniectomy has the potential to save lives, there are risks and consequences associated with procedure, including:
- Infection (wound infection, meningitis)
- Haemostasis development or bleeding
- Herniation of the brain or sinking flap syndrome
- Seizures
- Accumulation of fluid under the scalp
- Deformity for cosmetic purposes (till cranioplasty is done)
Depending on the patient’s condition, the procedure’s timing, and its purpose, reported complication rates range from 10% to 30%.
The Consenting Process
Since most patients are unconscious or in severe condition, the patient’s family is asked for their complete informed permission prior to the procedure.
The neurosurgical team discusses throughout this procedure:
- The surgery’s goal (to preserve life or stop more brain injury)
- The potential results (ranging from complete recovery to severe disability)
- The possible issues
- Future surgery (cranioplasty) is required.
- The prognosis and requirements for rehabilitation
To ensure that the choice is made completely and clearly, the family is invited to express any questions they may have.
Other Surgical Types and Alternative Options
Before choosing a decompressive craniectomy in some circumstances, medical professionals may think about or combine additional treatments like:
- Ventriculostomy (External Ventricular Drain, or EVD): To relieve pressure and drain cerebrospinal fluid, a tiny catheter is placed into the brain’s ventricles.
- Medical management may involve anaesthesia, hypothermia, controlled breathing, or hyperosmolar treatment (mannitol, hypertonic saline).
- Shunt Surgery: To redirect fluid from the brain to another body cavity in cases of chronic hydrocephalus or persistent cerebrospinal fluid accumulation, a shunt may be implanted.
- Decompressive Hemicraniectomy: When a big stroke occurs, one side of the skull is removed.
- Decompression of the posterior fossa is performed to treat swelling in the brainstem or cerebellum.
The neurosurgeon always discusses all viable options and expected outcomes to take an informed opinion from the patient’s family.
The Outlook
There is a substantial chance of death. This is due to the fact that the injuries that need this procedure are almost always deadly. Despite the procedure, many people do not survive. However, the majority of people have a better chance of living longer and experiencing fewer disabilities after having a craniectomy.
People who had decompressive craniectomy and those who received other medical treatments for brain edema were compared in a 2016 study.
According to the study, 26.9 percent of patients who had surgery had passed away six months after the procedure, compared to 48.9 percent of those who did not. Compared to 34.6 percent of the non-surgical group, 42.8 percent of the surgery group’s physicians classified the results as “favourable.”
Although there were significant rates of disability in both groups, the rate of all types of disability was reduced with decompressive craniectomy. For example, at 6 months, 2.1 percent of those who had surgery were in a vegetative state, whereas 8.5 percent of those who did not.
Conclusion
It can be scary to have a decompressive craniectomy. However, patients should be aware that the major cause of the high rate of post-operative complications is the severe injuries that required surgery. A craniectomy might be the best and only course of action for patients with severe edema that does not improve using standard therapies.
Some people may be able to resume their regular life after this procedure with the help of intensive rehabilitation care, close medical supervision, and timely treatment of any difficulties.
Source:
- https://pmc.ncbi.nlm.nih.gov/articles/PMC6517544/
- https://pubmed.ncbi.nlm.nih.gov/18392785/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC4771225/
- https://www.medicalnewstoday.com/articles/319755#takeaway
- https://www.physio-pedia.com/Decompressive_Craniectomy_(DC)
- https://www.sciencedirect.com/topics/medicine-and-dentistry/decompressive-craniectomy
- https://www.nejm.org/doi/full/10.1056/NEJMoa1605215#t=article
Craniotomy: During surgery, a bone flap is momentarily removed and then reinserted to remove a tumour or clot.