Topics
Table of Contents
The inability to move the muscles on one or both sides of your face as a result of nerve injury is known as facial paralysis. Inflammation, trauma, stroke, or tumours are among the potential reasons. The underlying illness that caused the paralysis determines the course of treatment. Both temporary and permanent facial paralysis are possible.
It can be divided into two categories according to where the incidental pathology occurs:
➜Palsy in the central face
Because of damage above the nucleus of the face
➜Facial palsy on the periphery
Due to damage to the facial nucleus or underneath
The facial muscles do not receive the signals they require to perform correctly when a facial nerve is absent or non-functioning. This causes the affected section of the face to become paralysed, which may affect movement in the mouth, eye(s), and other parts of the face.
Facial paralysis can vary in severity; in certain situations, it affects only the lower portion of the face, in others, it affects one side of the face entirely, and in yet others, it affects both sides.
What is Facial Reanimation?

The term “facial reanimation” refers to a surgical operation or set of procedures used to restore facial movement. Surgery for facial paralysis or facial palsy can be of two types:
- When your face is at rest, static restoration makes the two sides appear more symmetrical. They don’t make your facial muscles move again.
- Dynamic restoration restores movement and makes your face appear more symmetrical. For example, this type of surgery can assist you in closing your eye or smile.
What is the process of facial reanimation?

Physicians can use a variety of surgical techniques and methods to treat facial palsy.
- Nerve repair: In rare cases, the injured facial nerve segment may be immediately repaired by the surgeon.
- Nerve graft: The surgeon may use healthy nerve tissue extracted from another part of the body to fuse the nerve ends if too much of the face nerve is injured. We refer to this process as a nerve transplant.
- Nerve transfer: Instead of fixing the damaged area of the facial nerve, the surgeon may choose to completely avoid it in some situations. A healthy donor nerve is chosen by the surgeon from another part of the body or face where it is redundant or otherwise not essential to any function in a technique called a nerve transfer.
Video Link: Facial reanimaon procedures- Prof Deepak Agrawal
Usually, these operations are carried out in stages.
- Blepharoplasty, weight placement in the upper lid, lower lid canthoplasty, and brow ptosis repair are examples of static solutions for the top face. Static solutions for the lower face (to reconstruct the smile) include midface lift techniques or fascial slings.
- Temporalis myoplasty, same side or cross face nerve grafting, free functional muscle transfer, and “babysitter” nerve transfer treatments are examples of dynamic reconstructive options.
- By “borrowing” functional redundant nerve branches from the normal side of the face, a surgeon can restore dynamic function to the paralysed side of the face through a cross-facial nerve graft. Allowing for a symmetrical smile with emotion is the aim of this procedure. The usual side’s functionality shouldn’t be impacted. For this treatment, a healthy donor nerve graft is also taken from the lower leg.
- Regional muscle transfer may be necessary if the damaged facial nerve branch’s function cannot be restored because the muscles it activates cannot move again. The temporalis muscle may be activated by the surgeon in this situation. To facilitate chewing, this muscle, which is found on the side of the skull, connects to the jaw bone. A smile can be restored by realigning the tendon that connects the temporalis muscle to the jaw to the lip.
- Similar to this, in a free functional muscle transfer, the surgeon removes a healthy muscular segment from the gracilis, an inner thigh muscle, where it is not required. After that, the surgeon replaces the facial muscles that aren’t working by transferring the muscle, together with its motor nerve and blood artery, to the face.
A patient’s quality of life is greatly impacted by facial paralysis, a debilitating disorder that affects speech, eye closure, facial expressions, and oral competence. Numerous factors, including as trauma, tumours, infections, and congenital conditions, can cause it. Through the use of microsurgical, nerve grafting, and muscle transfer techniques, facial reanimation treatments seek to restore the face’s symmetry and dynamic movement. A thorough examination of contemporary facial reanimation methods, their indications, and anticipated results is given in this article.
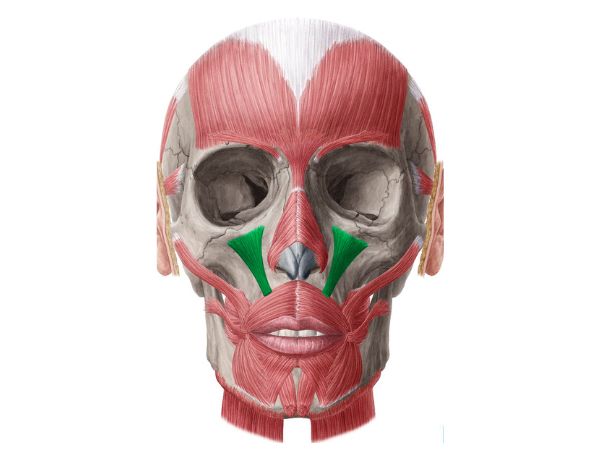
The Facial Nerve’s Anatomy:
After leaving the internal auditory canal and the stylomastoid foramen, the facial nerve (cranial nerve VII) splits into five terminal divisions: temporal, zygomatic, buccal, mandibular, and cervical. It is responsible for reflexes, autonomic processes, and voluntary facial motions.
The Cause of Paralysis of the Face
- Congenital causes: Congenital facial palsy, Moebius syndrome.
- Trauma: Iatrogenic injuries, temporal bone fractures
- Infections: Ramsay Hunt syndrome, Bell’s palsy
- Neoplasms: Parotid tumours, vestibular schwannomas.
- Iatrogenic Causes: Nerve damage following surgery
Classification of Paralysis of the Face
- Acute vs. Unremitting: Acute (less than six months), Chronic (more than six months)
- Complete vs. Inadequate: Based on useful impairment
- Unilateral vs. Respective: One-sided being more common
Techniques for Facial Reanimation
Procedures for Static Reanimation
Enhancing facial symmetry while at rest without restoring voluntary movement is the aim of static treatments.
- Suspension Techniques: Allografts or autologous fascia lata are used to create facial slings.
- Eyelid weights made of gold or platinum can help close the eyelids and shield the cornea.
- Tarsorrhaphy: Eyelids that are partially closed
- Using fillers or implants to contour the face: To enhance facial beauty
Procedures for Dynamic Reanimation
Dynamic procedures allow the paralysed face to move again.
Techniques Based on Nerves
- Primary repair of a transected facial nerve is known as direct neurorrhaphy.
- When direct repair is not feasible, sural or larger auricular nerve grafts are used.
- Hypoglossal-Facial Nerve Transfer: The hypoglossal nerve may transfer entirely or partially to the facial nerve.
- Masseteric-Facial Nerve Transfer: Reinnervation of the masseter muscle via the motor nerve
Methods Based on Muscles
- A portion of the temporalis muscle is transferred during a temporalis myoplasty to restore lip movement and eye closure.
- A two-stage microsurgical technique called gracilis free muscle transfer uses the gracilis muscle, which is innervated by the masseteric or contralateral facial nerve.
- Latissimus Dorsi Free Muscle Transfer: Used in complex situations when greater muscle mass is needed
Rehabilitation and Postoperative Care
For the best functional results after facial reanimation surgery, rehabilitation is essential. Important elements consist of:
- Physical therapy: Enhancing muscular tone using facial workouts
- Biofeedback methods for neuromuscular retraining to improve motor control
- Botulinum toxin therapy: used to enhance symmetry and lessen synkinesis
- Psychosocial Support: Handling the effects on the mind and emotions
Results and Outlook
The timing of the intervention, the level of nerve damage, the patient’s dedication to rehabilitation, and the surgeon’s expertise are some of the factors that affect the outcome of facial reanimation treatments. In general, better results come from early intervention. While dynamic operations restore voluntary mobility over the course of months to years, static procedures offer an instant visual enhancement.
Prospects for the Future
Some advancements in facial reanimation are:
- Investigating regenerative methods for nerve regeneration with stem cell therapy
- Improving the Accuracy of Reconstruction with 3D Printing and Custom Implants
- Increasing the precision of surgery with robotic-assisted microsurgery
- Examining molecular strategies for nerve regeneration with gene therapy
In conclusion
Although facial paralysis presents serious functional and cosmetic difficulties, face expression can be restored with the help of contemporary surgical procedures. For patients having face reanimation operations, the best results can be obtained through a multidisciplinary strategy that combines neurosurgery, plastic surgery, and rehabilitation.
Sources:
- https://www.mayoclinic.org/tests-procedures/facial-reanimation-surgery/about/pac-20556545
- https://www.barrowneuro.org/treatment/facial-reanimation/
- https://medicine.uiowa.edu/iowaprotocols/facial-reanimation
- https://pmc.ncbi.nlm.nih.gov/articles/PMC9143601/
- https://www.physio-pedia.com/Facial_Palsy
- https://www.facialpalsy.org.uk/inform/what-is-facial-palsy/