Topics of the week
Table of Contents
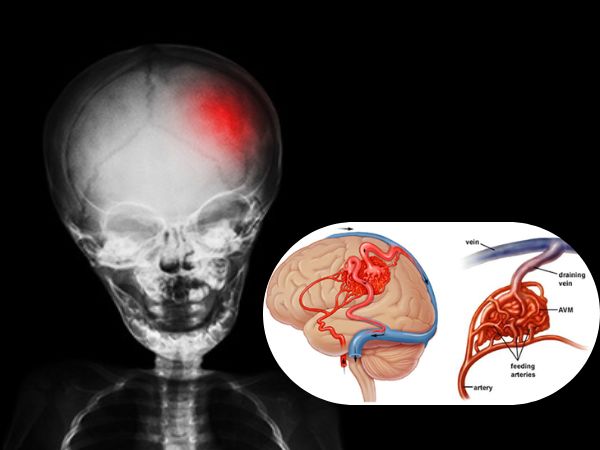
Rare but potentially dangerous brain vascular anomalies are called intracranial dural arteriovenous fistulas (dAVFs). They have to do with abnormal artery-vein connections in the dura mater, the brain’s outermost layer. In contrast to congenital arteriovenous malformations (AVMs), dAVFs are usually acquired lesions that may arise later in life as a result of venous thrombosis, trauma, infection, or surgery. Certain dAVFs might result in life-threatening bleeding or severe neurological impairments if treatment is not received.
A Dural Arteriovenous Fistula: What Is It?
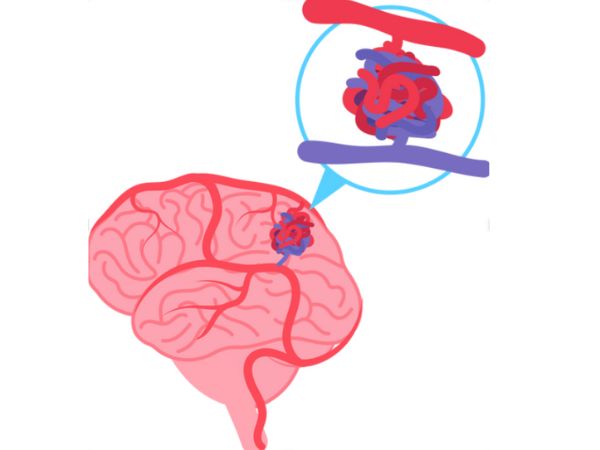
An irregular direct connection between the meningeal arteries and the dural venous sinuses or cortical veins is known as a dural arteriovenous fistula (dAVF). Blood normally travels from arteries to capillaries and finally to veins. This capillary bed is bypassed in a dAVF, allowing high-pressure arterial blood to enter the low-pressure venous system directly. Depending on the drainage pattern and location, this can cause neurological symptoms, venous congestion, or haemorrhage.
Reasons/Causes and Dangers
A number of factors are linked to the development of dAVFs, though their exact cause is not always evident:
- Thrombosis of the dural sinuses
- Head injuries
- Neurosurgical techniques
- Infections
- States of hypercoagulability
With no obvious gender preference, they are most frequently observed in middle-aged to older persons.
The symptoms of the Intracranial Dural Arterivenous Fistula are as follows:
The size, location, and blood flow pattern of dAVFs all affect the symptoms. While some may show up with serious neurological problems, others may stay asymptomatic and be found by chance.
Typical signs and symptoms include:
- A headache
- Hearing a rhythmic sound in the ear is known as pulsatile tinnitus.
- Visual disruptions
- Seizures
- Deficits in the cranial nerve
- Dementia-like symptoms or cognitive decline
- Haemorrhage inside the brain (in high-grade fistulas)
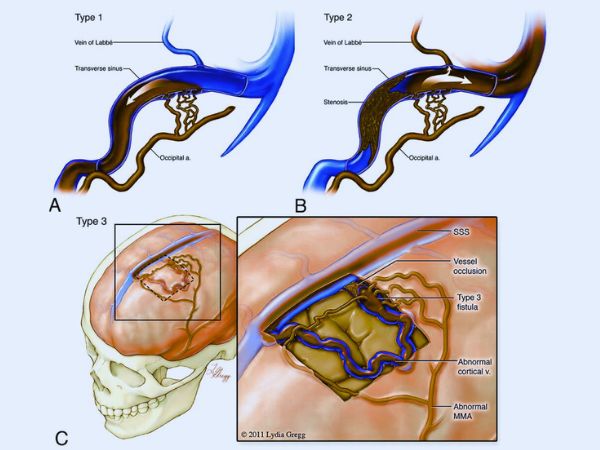
Classification
Based on their venous drainage patterns and haemorrhage risk, dAVFs are categorised using the Cognard and Borden categorisation systems.
Classification by Borden:
- Type I: Low risk drainage into a venous sinus
- Type II: Retrograde cortical venous drainage into a venous sinus (moderate risk)
- Type III: High-risk direct cortical venous drainage
Classification by Cognard:
Varies according to venous drainage patterns and flow direction, ranging from Type I (benign) to Type V (most aggressive).
Diagnosis
In order to avoid complications, early diagnosis is essential. The imaging modalities that are employed include:
- For preliminary evaluation, magnetic resonance imaging (MRI) and magnetic resonance angiography (MRA) are helpful.
- Computed Tomography Angiography (CTA): May reveal abnormal veins and swollen feeding arteries.
- The gold standard for diagnosis is digital subtraction angiography (DSA), which offers fine-grained visualisation of the venous drainage, feeding arteries, and fistula.
Options for Treatment
The dAVF’s categorisation, location, and symptoms all influence the therapy option. The goal of treatment is to restore normal venous drainage and close the abnormal link.
Embolisation of Endovascular
- A minimally invasive procedure in which the fistula is sealed shut by administering embolic chemicals via a catheter.
- Frequently the initial course of treatment.
Resection by Microsurgery
- Used when embolisation is impractical or fails.
- Involves cutting the fistula directly during surgery.
Gamma Knife Surgery, or stereotactic radiosurgery
- An approach for non-invasive therapy that works especially well for residual or low-flow fistulas.
Intracranial Dural Arteriovenous Fistulas with Gamma Knife Surgery
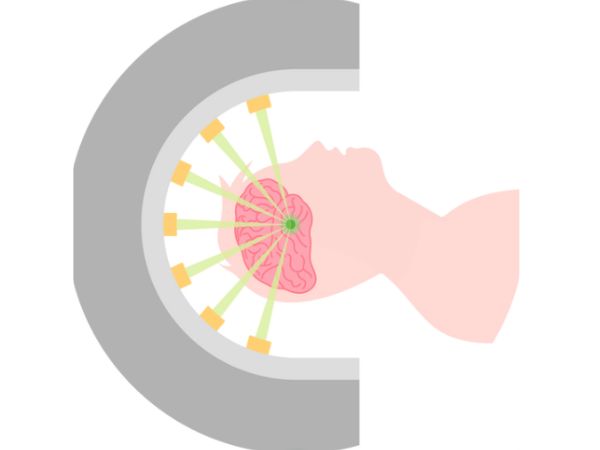
A type of stereotactic radiosurgery known as “gamma knife” (GKS) uses concentrated, high-dose radiation beams to precisely target the abnormal vascular connections inside the dura while preserving the surrounding healthy brain tissue.
How It Operates:
- Through damage to endothelial cells and vessel wall thickening, the radiation causes the unusual vessels to gradually close over the course of months to years.
- It is usually applied to individuals who are not a good candidate for invasive procedures or to low-grade or persistent dAVFs following unsuccessful embolisation.
Gamma Knife Surgery Indications for dAVFs:
- Tiny, persistent fistulas following embolisation
- Deeply seated or inaccessible surgical sites
- Low-risk dAVFs that are asymptomatic or only slightly symptomatic
- Comorbidities in patients that raise the risk of surgery
Benefits:
- Non-invasive
- Procedure for outpatients
- Short recovery period
- Suitable for use in conjunction with additional therapies
Limitations:
- Effect delayed: Total obliteration may take six to thirty-six months.
- Not appropriate for high-grade or quickly developing fistulas with cortical venous reflux.
- The evaluation of obliteration requires routine follow-up imaging.
Prognosis and Follow-Up
The fistula’s classification and drainage pattern determine the prognosis. While low-risk dAVFs can be seen, high-risk ones need to be treated right away.
Follow-up consists of:
- DSA or serial MRI/MRA
- Preventing recurrence
- Neurological evaluation
In most situations, a favourable outcome can be achieved with appropriate diagnosis and treatment. For certain cases, Gamma Knife Surgery has demonstrated exceptional obliteration rates with little adverse consequences.
In conclusion
Vascular abnormalities known as intracranial dural arteriovenous fistulas are complicated but curable. For the best results, a multidisciplinary strategy including radiation oncologists, neurosurgeons, and interventional neuroradiologists is essential. For some forms of dAVFs, Gamma Knife Surgery has become a potent non-invasive treatment option, particularly when embolisation or traditional surgery may be unsafe or insufficient.
Early contact with a specialised neurosurgery team can significantly impact treatment outcomes and quality of life if you or a loved one is diagnosed with a dAVF.
Sources:
- https://pmc.ncbi.nlm.nih.gov/articles/PMC8013238/#sec10
- https://pmc.ncbi.nlm.nih.gov/articles/PMC5435465/
- https://radiopaedia.org/articles/dural-arteriovenous-fistula
- https://www.ahajournals.org/doi/10.1161/strokeaha.115.008228
- https://my.clevelandclinic.org/health/diseases/dural-arteriovenous-fistula-davf
- https://www.mayoclinic.org/diseases-conditions/dural-arteriovenous-fistulas/symptoms-causes/syc-20364280
- https://link.springer.com/article/10.1007/s13760-022-02133-6
You May Also Know Related to Gamma Knife
FAQ’s
How does Gamma Knife work?
Gamma Knife uses 192–201 precisely focused beams of gamma rays that converge at a single target point in the brain. This high dose of radiation damages the DNA of abnormal cells, stopping their growth or causing them to shrink, while minimizing exposure to nearby healthy tissue.
Is Gamma Knife a surgery?
No, Gamma Knife is not a traditional surgery. It is a non-invasive outpatient procedure performed without any incision, stitches, or general anesthesia in most cases.
What conditions can be treated with Gamma Knife?
Gamma Knife is commonly used for:
Brain tumors (benign and malignant)
Metastatic brain lesions
Arteriovenous malformations (AVMs)
Trigeminal neuralgia
Acoustic neuromas (vestibular schwannomas)
Pituitary tumors
Certain functional disorders (like tremors)
Is Gamma Knife painful?
The procedure is generally painless. Patients may feel mild pressure while the head frame (if used) is applied or may experience slight discomfort from anesthesia injections, but the treatment itself is not painful.
How long does the procedure take?
Depending on the condition and treatment plan, Gamma Knife may take 30 minutes to 3 hours. Most patients go home the same day.
What are the possible side effects?
Common side effects are usually mild and temporary, including:
Headache
Nausea
Fatigue
Mild scalp swelling or tenderness at the frame site
Rarely, some patients may experience delayed radiation effects such as brain swelling or radiation necrosis.
When can the patient return to normal activities after Gamma Knife?
Most patients can return to their normal routine within 24–48 hours after the procedure.
You may feel mild fatigue for a few days.
Follow-up imaging is usually required after 1 year.
How effective is Gamma Knife?
Gamma Knife has a high success rate and has been used worldwide for decades. Its effectiveness depends on the condition treated, size and location of the lesion, and overall patient health. In many cases, it offers results comparable to open surgery with fewer risks.
Can Gamma Knife be repeated if needed?
Yes, in some cases Gamma Knife treatment can be repeated if the disease recurs or if new lesions develop.
Is Gamma Knife safe?
Yes. Gamma Knife is considered one of the safest and most precise forms of radiosurgery, with millions of patients treated globally and extensive clinical data supporting its use.
Who is eligible for Gamma Knife treatment?
Eligibility depends on factors such as:
Size and location of the lesion
Overall health and age
Whether open surgery is too risky
A neurosurgeon and radiation oncologist will decide if Gamma Knife is the best option for you.
What happens before the procedure?
A detailed MRI or CT scan is performed to map the brain.
A lightweight head frame or mask is used for accuracy.
Your doctors plan the radiation dose and target areas using specialized software.
Will I need anesthesia?
Local anesthesia is given if a head frame is used.
General anesthesia is usually not required, except for children or patients unable to remain still.
What is the cost of Gamma Knife in India?
Costs vary depending on hospital, city, and condition treated. On average, Gamma Knife in India ranges from ₹1.5 lakh to ₹4.5 lakh. It is usually more affordable compared to treatment in Western countries. At AIIMS Delhi, it is much more affordable around ₹75,000 which makes it affordable for the patients in need.
Where can I get Gamma Knife treatment in Delhi?
AIIMS Delhi is one of the leading centres for Gamma Knife in India.
AIIMS uses the latest Gamma Knife Perfexion system.
It has successfully treated thousands of patients for brain tumors, blood vessel problems, and even eye cancers.
The treatment is done by expert neurosurgeons such as Dr. Deepak Agrawal and team.
Clinic timings for Gamma Knife OPD at AIIMS Delhi: Monday & Friday, 8:00 AM – 9:00 AM.
Cost is around ₹75,000 and is subsidized compared to private hospitals.
What is the complete process of the Gamma Knife?
The whole procedure is usually done in one day:
- Consultation & Planning – Doctors review your scans and decide the treatment.
- Head Frame/Mask – A lightweight frame or mask is placed to keep your head still.
- Imaging – MRI/CT scans are done to locate the exact target.
- Treatment Planning – Specialists plan the dose and direction of radiation.
- Gamma Knife Treatment – You lie on the machine; painless radiation beams treat the target (30 mins–3 hrs).
- Recovery & Discharge – The frame is removed, and most patients go home the same day.
- Follow-up – MRI after a few months to check results.
What formalities do I have to complete prior to getting the date of GK?
Before you get a treatment date, you need to complete a few steps:
- OPD Registration – Visit the Neurosurgery OPD (Gamma Knife clinic at AIIMS, Mon & Fri 8–9 AM) and register.
- Consultation with Doctor – Meet the neurosurgeon who will check your reports, MRI/CT scans, and medical history.
- Investigations – Sometimes fresh MRI/CT or blood tests are needed for treatment planning.
- Medical Fitness – Basic checks like blood pressure, sugar, heart condition, etc.
Financial/Insurance Approval –
- If using Ayushman Bharat or government schemes, you need approval papers.
- If self-paying, you will be given the estimated cost (~₹75,000 at AIIMS).
- Consent & Admission Slip – Once doctors confirm you are fit and formalities are done, you sign the consent form.
- Treatment Date Allotment – A date is given for your Gamma Knife procedure.
What formalities do I have to complete after getting the date of GK?
Once you receive your Gamma Knife date, you’ll need to do a few simple things before the procedure:
- Admission Process – Report to AIIMS on the morning of your procedure and complete admission at the Neurosurgery ward/Daycare.
- Paperwork – Carry your OPD slip, MRI/CT films, blood test reports, admission slip, and ID proof. If you are covered under Ayushman Bharat/insurance, keep those approval papers ready.
- Consent Forms – You (or a family member) will sign consent for the procedure and anesthesia.
- Medical Check-up – Doctors will check your BP, sugar, heart rate, and do a quick physical exam.
- Fasting – Usually, you will be asked to not eat or drink for 6 hours before the procedure.
- Pre-Procedure Prep – An IV line may be put, and medicines (sedation/antibiotics if needed) are given.
- Treatment – You are then taken to the Gamma Knife room for frame/mask placement, imaging, and treatment.
After the procedure, you’ll be observed for a few hours and most patients are discharged the same day or next morning.
What investigations to be done?
Urea & creatinine
Should I come fasting?
No, You can have light breakfast.
In case of HT/DM should take my medicines?
Yes, you can take the medicine and then come for the treatment.
