Topics
Table of Contents
Craniopharyngioma: What is it?
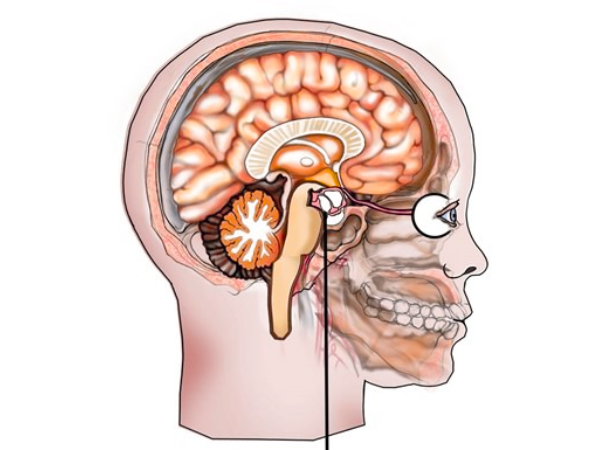
An important medical problem that may necessitate lifelong care is a craniopharyngioma. Over time, almost half of all surgically excised tumours recur. Numerous illnesses brought on by craniopharyngiomas persist even after the tumour has been removed.
What distinguishes a pituitary adenoma from a craniopharyngioma?
Hormone function can be impacted by pituitary adenomas and craniopharyngiomas. Craniopharyngiomas are found close to the pituitary gland, while pituitary adenomas are tumours that originate from the pituitary gland itself. Despite the fact that both tumours are benign, pituitary adenomas are often less aggressive than craniopharyngiomas.
Histology and Types
Two primary histological subtypes exist:
- Children are more likely to have Adamantinomatous Craniopharyngioma (ACP). characterised by calcifications, cystic components, and frequently a more infiltrative character.
- PCP, or papillary craniopharyngioma, is usually observed in adults. less calcified and more firm, frequently leading to superior surgical results.
Pathogenesis and Causes
Although the precise source is unknown, it is believed that craniopharyngiomas develop from the remains of Rathke’s pouch, an embryonic structure that gives birth to the anterior pituitary.
- Mutations in the CTNNB1 gene (β-catenin pathway) are frequently linked to the amantinomatous type.
- BRAF V600E mutations have therapeutic implications and are associated with papillary type.
Signs and symptoms
Because craniopharyngiomas are located close to important brain areas, they can cause a range of symptoms:
- Visual abnormalities (caused by the optic chiasm being compressed)
- A headache
- Imbalances in hormones (causd by pituitary malfunction)
- Children’s growth delays
- Fatigue, memory problems, and obesity (because of hypothalamus involvement)
- If the tumour blocks the cerebrospinal fluid channels, hydrocephalus may result.
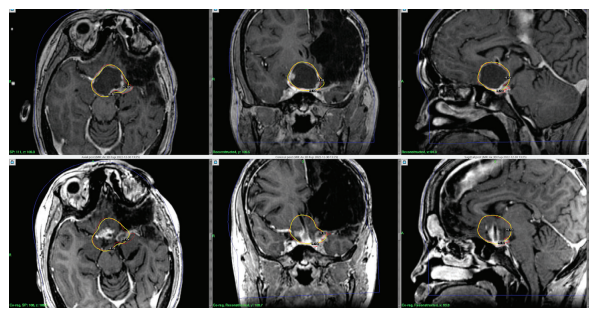
Diagnosis
- Imaging:
- The gold standard is MRI, which shows calcifications, cystic/solid mass, and the connection to surrounding structures.
- A CT scan can make calcifications easier to see.
- Endocrine Assessment:
- Pituitary hormone testing, both baseline and dynamic, is crucial.
Options for Treatment
A comprehensive approach is necessary for the management of craniopharyngiomas. Maximum tumour control while maintaining neurological and endocrine function is the aim.
Surgery
The standard of care is still surgical removal. Methods consist of:
- Craniotomy, or transcranial surgery
- For midline lesions, the endoscopic endonasal approach (EEA) is becoming more and more popular.
Adherence to key structures may make complete excision difficult.
Radiation therapy
Radiotherapy after surgery is frequently used when:
- The tumour has been partially removed.
- Recurrence happens.
- Surgery is very risky.
Proton treatment, stereotactic radiosurgery, and conventional fractionated radiation are available.
Radiosurgery with Gamma Knife for Craniopharyngiomas
Gamma Knife Radiosurgery: What is it?
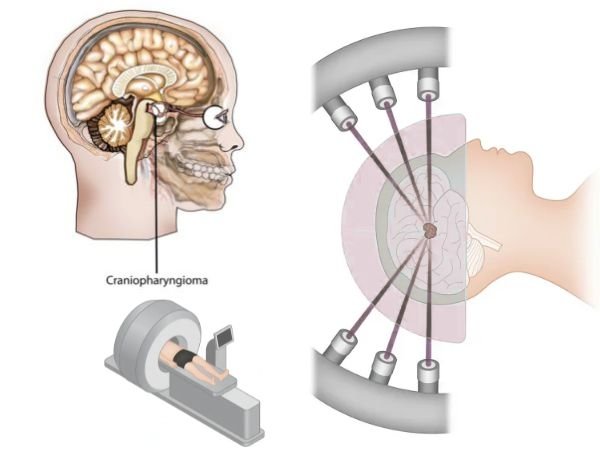
Gamma Knife radiosurgery is a non-invasive stereotactic procedure that spares the surrounding brain tissue while precisely giving high doses of radiation to the tumour. Small to medium-sized lesions close to important structures respond especially well to treatment.
Indications or Signs and symptoms of craniopharyngiomas
- After subtotal resection, residual tumour
- Recurrence following the initial procedure
- Patients who are medically inoperable
- Near optical equipment, tumours (with appropriate dose planning)
- Before GKRS, cystic components may be shrunken or aspirated.
Craniopharyngioma Primary Gamma Knife Radiosurgery
Gamma Knife radiosurgery can be used as the main treatment in some circumstances without surgical resection, especially in:
- Tumours that are little (<3 cm)
- Clearly clear margins
- Tumours that don’t produce immediate symptoms like hydrocephalus or profound blindness
- Patients in poor overall health or at high risk for surgery
Benefits:
- Minimally intrusive or invasive
- Maintains brain function
- Outpatient treatment or brief hospitalisation
- Shorter recuperation period
- Repeatable if necessary
Restrictions:
- Large, symptomatic, or cystic tumours with mass effect are not the best candidates.
- Risk of visual deterioration or delayed hypopituitarism (rare with proper dose)
Results and Outlook
It is possible to achieve long-term tumour control with the right care. But even after treatment, endocrine dysfunction frequently continues. Hormonal testing and MRI imaging are necessary for lifelong monitoring.
Rates of Survival:
- Overall 5-year survival: greater than 90%
- In carefully chosen patients, the Gamma Knife tumour control rate is 80–90%.
In conclusion
Despite being benign, craniopharyngiomas present a number of difficulties because of their location and effect on essential activities. The greatest results are guaranteed by a customised strategy that combines stereotactic radiosurgery, such as Gamma Knife, radiation, and surgery. Primary Gamma Knife radiosurgery is a safe and efficient substitute for surgery in carefully selected patients, particularly where neurological and endocrine function preservation is the goal.
Sources:
- https://www.ncbi.nlm.nih.gov/books/NBK459371/#:~:text=Craniopharyngioma%20is%20a%20rare%2C%20virtually,visual%20disturbances%2C%20and%20endocrine%20disturbances.
- https://www.mayoclinic.org/diseases-conditions/craniopharyngioma/symptoms-causes/syc-20581521
- https://my.clevelandclinic.org/health/diseases/22989-craniopharyngioma
- https://en.wikipedia.org/wiki/Craniopharyngioma
- https://www.hopkinsmedicine.org/health/conditions-and-diseases/craniopharyngioma
- https://www.aans.org/patients/conditions-treatments/craniopharyngiomas/
- https://academic.oup.com/edrv/article-abstract/27/4/371/2355225?redirectedFrom=fulltext
- https://www.sciencedirect.com/science/article/pii/S0003426624001082
You May Also Know Related to Gamma Knife
FAQ’s
How does Gamma Knife work?
Gamma Knife uses 192–201 precisely focused beams of gamma rays that converge at a single target point in the brain. This high dose of radiation damages the DNA of abnormal cells, stopping their growth or causing them to shrink, while minimizing exposure to nearby healthy tissue.
Is Gamma Knife a surgery?
No, Gamma Knife is not a traditional surgery. It is a non-invasive outpatient procedure performed without any incision, stitches, or general anesthesia in most cases.
What conditions can be treated with Gamma Knife?
Gamma Knife is commonly used for:
Brain tumors (benign and malignant)
Metastatic brain lesions
Arteriovenous malformations (AVMs)
Trigeminal neuralgia
Acoustic neuromas (vestibular schwannomas)
Pituitary tumors
Certain functional disorders (like tremors)
Is Gamma Knife painful?
The procedure is generally painless. Patients may feel mild pressure while the head frame (if used) is applied or may experience slight discomfort from anesthesia injections, but the treatment itself is not painful.
How long does the procedure take?
Depending on the condition and treatment plan, Gamma Knife may take 30 minutes to 3 hours. Most patients go home the same day.
What are the possible side effects?
Common side effects are usually mild and temporary, including:
Headache
Nausea
Fatigue
Mild scalp swelling or tenderness at the frame site
Rarely, some patients may experience delayed radiation effects such as brain swelling or radiation necrosis.
When can the patient return to normal activities after Gamma Knife?
Most patients can return to their normal routine within 24–48 hours after the procedure.
You may feel mild fatigue for a few days.
Follow-up imaging is usually required after 1 year.
How effective is Gamma Knife?
Gamma Knife has a high success rate and has been used worldwide for decades. Its effectiveness depends on the condition treated, size and location of the lesion, and overall patient health. In many cases, it offers results comparable to open surgery with fewer risks.
Can Gamma Knife be repeated if needed?
Yes, in some cases Gamma Knife treatment can be repeated if the disease recurs or if new lesions develop.
Is Gamma Knife safe?
Yes. Gamma Knife is considered one of the safest and most precise forms of radiosurgery, with millions of patients treated globally and extensive clinical data supporting its use.
Who is eligible for Gamma Knife treatment?
Eligibility depends on factors such as:
Size and location of the lesion
Overall health and age
Whether open surgery is too risky
A neurosurgeon and radiation oncologist will decide if Gamma Knife is the best option for you.
What happens before the procedure?
A detailed MRI or CT scan is performed to map the brain.
A lightweight head frame or mask is used for accuracy.
Your doctors plan the radiation dose and target areas using specialized software.
Will I need anesthesia?
Local anesthesia is given if a head frame is used.
General anesthesia is usually not required, except for children or patients unable to remain still.
What is the cost of Gamma Knife in India?
Costs vary depending on hospital, city, and condition treated. On average, Gamma Knife in India ranges from ₹1.5 lakh to ₹4.5 lakh. It is usually more affordable compared to treatment in Western countries. At AIIMS Delhi, it is much more affordable around ₹75,000 which makes it affordable for the patients in need.
Where can I get Gamma Knife treatment in Delhi?
AIIMS Delhi is one of the leading centres for Gamma Knife in India.
AIIMS uses the latest Gamma Knife Perfexion system.
It has successfully treated thousands of patients for brain tumors, blood vessel problems, and even eye cancers.
The treatment is done by expert neurosurgeons such as Dr. Deepak Agrawal and team.
Clinic timings for Gamma Knife OPD at AIIMS Delhi: Monday & Friday, 8:00 AM – 9:00 AM.
Cost is around ₹75,000 and is subsidized compared to private hospitals.
What is the complete process of the Gamma Knife?
The whole procedure is usually done in one day:
- Consultation & Planning – Doctors review your scans and decide the treatment.
- Head Frame/Mask – A lightweight frame or mask is placed to keep your head still.
- Imaging – MRI/CT scans are done to locate the exact target.
- Treatment Planning – Specialists plan the dose and direction of radiation.
- Gamma Knife Treatment – You lie on the machine; painless radiation beams treat the target (30 mins–3 hrs).
- Recovery & Discharge – The frame is removed, and most patients go home the same day.
- Follow-up – MRI after a few months to check results.
What formalities do I have to complete prior to getting the date of GK?
Before you get a treatment date, you need to complete a few steps:
- OPD Registration – Visit the Neurosurgery OPD (Gamma Knife clinic at AIIMS, Mon & Fri 8–9 AM) and register.
- Consultation with Doctor – Meet the neurosurgeon who will check your reports, MRI/CT scans, and medical history.
- Investigations – Sometimes fresh MRI/CT or blood tests are needed for treatment planning.
- Medical Fitness – Basic checks like blood pressure, sugar, heart condition, etc.
Financial/Insurance Approval –
- If using Ayushman Bharat or government schemes, you need approval papers.
- If self-paying, you will be given the estimated cost (~₹75,000 at AIIMS).
- Consent & Admission Slip – Once doctors confirm you are fit and formalities are done, you sign the consent form.
- Treatment Date Allotment – A date is given for your Gamma Knife procedure.
What formalities do I have to complete after getting the date of GK?
Once you receive your Gamma Knife date, you’ll need to do a few simple things before the procedure:
- Admission Process – Report to AIIMS on the morning of your procedure and complete admission at the Neurosurgery ward/Daycare.
- Paperwork – Carry your OPD slip, MRI/CT films, blood test reports, admission slip, and ID proof. If you are covered under Ayushman Bharat/insurance, keep those approval papers ready.
- Consent Forms – You (or a family member) will sign consent for the procedure and anesthesia.
- Medical Check-up – Doctors will check your BP, sugar, heart rate, and do a quick physical exam.
- Fasting – Usually, you will be asked to not eat or drink for 6 hours before the procedure.
- Pre-Procedure Prep – An IV line may be put, and medicines (sedation/antibiotics if needed) are given.
- Treatment – You are then taken to the Gamma Knife room for frame/mask placement, imaging, and treatment.
After the procedure, you’ll be observed for a few hours and most patients are discharged the same day or next morning.
What investigations to be done?
Urea & creatinine
Should I come fasting?
No, You can have light breakfast.
In case of HT/DM should take my medicines?
Yes, you can take the medicine and then come for the treatment.
