Topics
Table of Contents
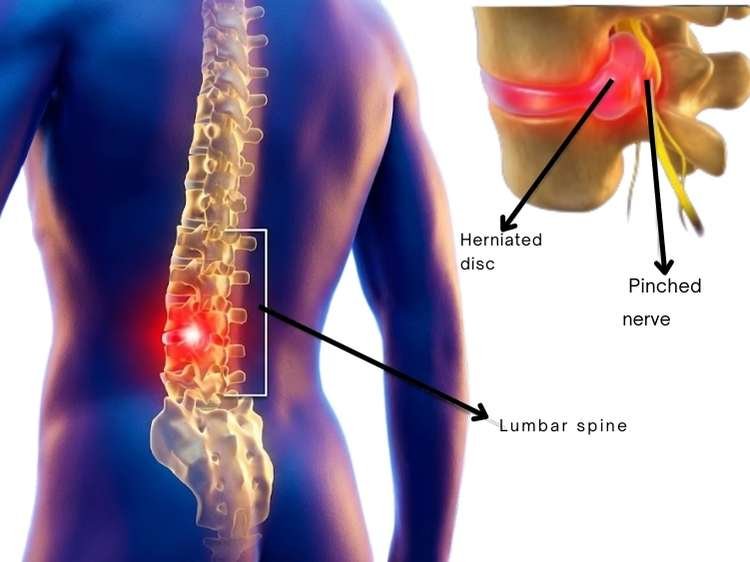
One of the most popular spine surgeries in the world is lumbar discectomy. It is intended to treat sciatica, or leg pain, and nerve compression brought on by a lower back herniated disc. In addition to providing answers to frequently asked concerns by patients and their families, this article describes the procedure, when it is necessary, viable alternatives, potential hazards, and the consenting process.
Lumbar Discectomy: What Is It?
A lumbar discectomy is a surgical technique used to remove a damaged or herniated portion of a lower back disc. A bulging or ruptured disc may put pressure on surrounding nerves, leading to:
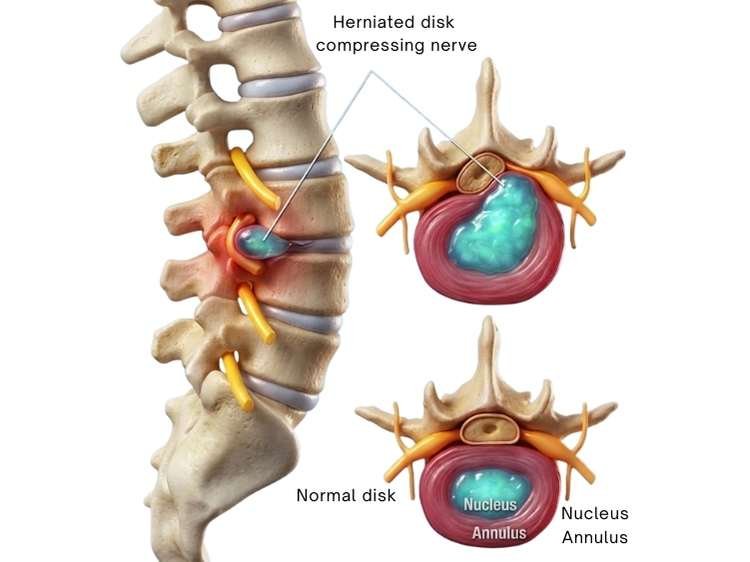
- Shooting or sharp sciatica, or leg discomfort
- Tingling or numbness
- Weakness in the foot or leg
- Having trouble standing or walking
- Pain radiating downward from the back
By relieving pressure on the compressed nerve, the operation aims to improve movement and lessen pain.
Why Is a Lumbar Discectomy Required?
A lumbar discectomy may be recommended by a neurosurgeon if:
- Despite medication, rest, and physical therapy, the pain lasts longer than six to twelve weeks.
- The leg is becoming more weaker.
- Walking, sitting, and sleeping are all negatively impacted.
- Disc herniation-related nerve compression is confirmed by MRI.
- Foot drop is one sign of nerve injury.
- Cauda equina syndrome rarely requires emergency surgery (loss of bladder/bowel control, saddle anaesthesia).
Lumbar Discectomy Types
Standard Lumbar Discectomy (Open)
- A tiny cut is made at the rear.
- To reach the spine, muscles are gradually retracted.
- The piece of herniated disc is extracted.
- Widely used and safe
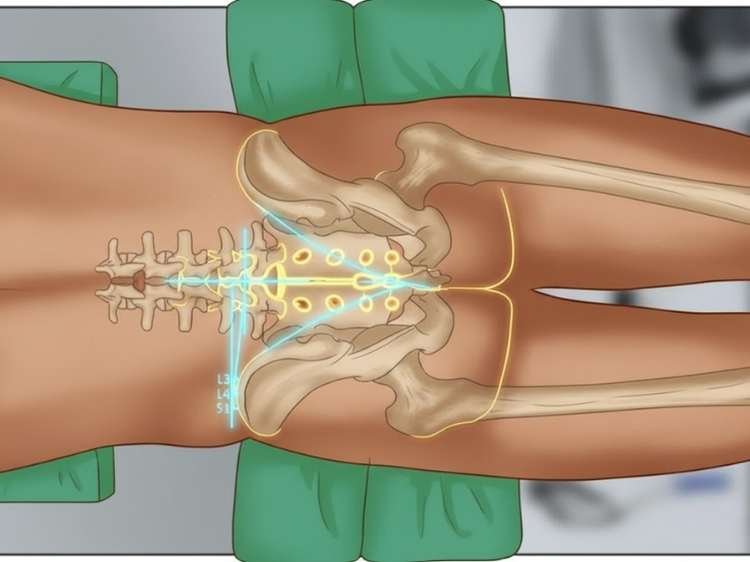
Minimally Invasive Microdiscectomy
- Carried out under a microscope
- Less muscle injury and a smaller incision
- Reduced surgical pain and a quicker recovery
- In contemporary spine surgery, it is frequently recommended
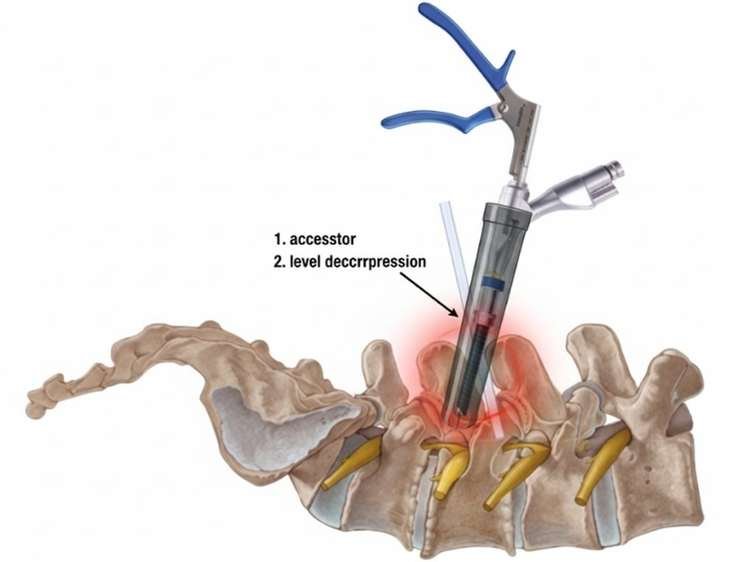
Discectomy via endoscopy
- Performed using instruments and a little camera
- Short-term procedure, nursery or minimal incision
- Not appropriate for every kind of disc herniation
What Takes Place During the Procedure?
- Carried out while under general anaesthesia
- Usually takes 45 to 90 minutes.
- The herniated disc fragment pushing on the nerve is removed by the surgeon.
- The disc that remains is kept intact.
- Typically, the patient walks the same day or the following day.
- Usually, discharge occurs in 24 to 48 hours.
Recuperation Following Lumbar Discectomy
- Anticipated Timeframe
- Walk the same day or the following day.
- Resuming light activity in two to four weeks
- Return to work in the office: four to six weeks
- For six weeks, refrain from lifting, bending, or twisting.
- Full recovery: 8–12 weeks
Included in Rehabilitation
- Physical therapy
- Exercises that strengthen the core
- Adjusting your posture
- Controlling weight
- Workplace and household ergonomics guidelines
Rate of Complications and Dangers
Over 90–95% of patients report significant ease from lumbar discectomy, which is regarded as a safe and successful treatment.
But like any surgery, there are potential dangers involved:
Common but insignificant hazards
- Pain at the location of the incision
- Light bleeding
- Momentary tingling or numbness
Less frequent hazards
- Dural tears (1–5%) may result in a CSF leak that can be fixed via surgery.
- Infection (1–2%) Rare when using antibiotics and sterile methods
- Nerve damage (<1%) Very uncommon
- Recurrent herniation of the disc (5–10%) The same disc may later re-herniate
- Blood clot is extremely uncommon.
During the consenting procedure, your surgeon will go over these risks with you.
What Patients and Their Families Need to Know About the Consenting Process
Prior to surgery, the physician will clarify:
The diagnosis
- MRI results
- The degree of nerve compression
- Relationship to symptoms
The Need for Surgery
- Conservative treatment’s failure
- Delay could result in irreversible nerve injury.
Plan for Surgery
- Discectomy type
- Anticipated outcomes
- Length of stay
Advantages versus Dangers
- Pain reduction
- An increase in mobility
- Potential issues (described above)
Other Treatment Options and Alternatives
- Before providing informed permission, families must be aware of all available options.
Alternative Therapies (Non-Surgical Choices)
Surgery is not always necessary for disc herniations. Other options consist of:
Drugs
- NSAIDs, or anti-inflammatory medications
- Relaxants for muscles
- Neuropathic painkillers
- Physical treatment
- Exercises for strengthening
- Traction (in certain situations) and postural training
- Injections of Epidural Steroids
- Decreases nerve-related inflammation
- Beneficial for mild symptoms
- Temporary relief is possible.
- Changes in Lifestyle
- Loss of weight
- Changes in ergonomics
- Strengthening of the core
- Heat/Cold Treatment
- Helps lessen pain and spasms in the muscles
- Only in cases of neurological deficiency or when all other measures have failed surgery is advised.
Related Post: Lumbar Spondylosis: Causes, Symptoms, and Treatments
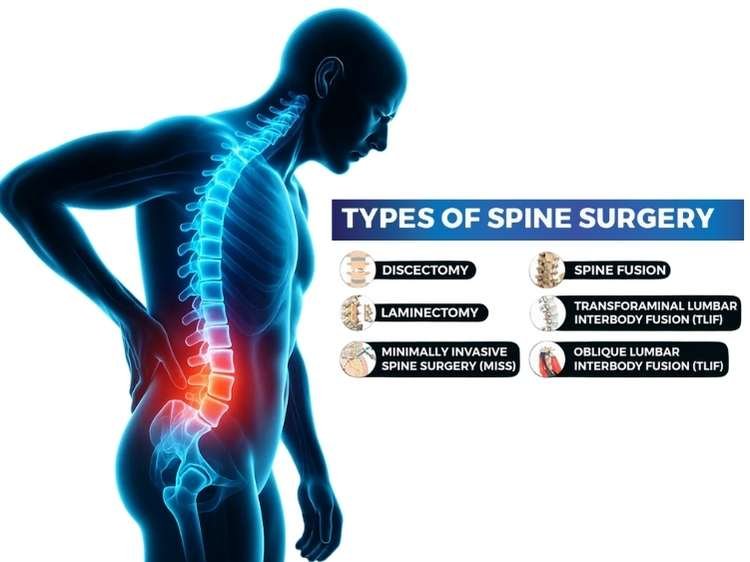
Other Surgical Procedures (Discectomy Excluded)
Depending on the severity and stability of the spine, the doctor may occasionally recommend additional procedures:
Laminectomy
- Removal of the lamina, a portion of the bone, to relieve pressure in cases of spinal stenosis.
Foraminotomy
- Reduces compression by widening the nerve exit canal.
Surgery for Fusion
- If there are several recurrent herniations, spondylolisthesis, or instability.
(Note: Shunt surgery is not utilised to cure disc herniation because it is used to treat hydrocephalus and has nothing to do with lumbar disc disease.)
In conclusion
For individuals with nerve compression brought on by a herniated disc, lumbar discectomy is a very successful treatment. Recovery is quicker, pain alleviation is substantial, and problems are rare with contemporary minimally invasive procedures.
All risks, advantages, and options should be considered before making a decision, though, to ensure that the patient and their family have given their informed permission.
FAQ’s
- Is a lumbar discectomy considered a major surgical procedure?
It is regarded as a minor to moderate procedure with a quick recovery time and a high success rate.
- Will the discomfort subside right away following surgery?
Usually, leg pain goes away right away. It takes a few days to weeks for back pain.
- Is it possible for the disc to slip again?
Indeed, the same disc may herniate again in 5–10% of patients.
- What is the duration of my hospital stay?
In minimally invasive circumstances, most patients are released the same day or stay for one to two days.
- When can I go back to work?
Light work: four to six weeks
8–12 weeks of intense physical labour
- Do I require physical therapy?
Indeed. For a complete recovery, a systematic rehabilitation program is necessary.
- Can elderly patients safely use it?
Sure, if you’re in good health. Safety is ensured by pre-operative evaluation.
- Will I be scarred?
Particularly in microdiscectomy, incisions are typically tiny. Scars diminish with time.
- What happens if I don’t get surgery?
In extreme situations, nerve damage may become irreparable, and pain may continue or intensify.
- After surgery, are I able to move, travel, or climb stairs?
Walking is encouraged, yes. For four to six weeks, stay away from lengthy rides and strenuous activity.
Sources:
- https://mayfieldclinic.com/pe-lumdiscectomy.htm
- https://www.nuffieldhealth.com/treatments/lumbar-discectomy
- https://neurosurgeondublin.ie/lumbar-discectomy-decompression/
- https://my.clevelandclinic.org/health/procedures/discectomy
- https://www.hopkinsmedicine.org/health/treatment-tests-and-therapies/minimally-invasive-lumbar-discectomy
- https://www.materprivate.ie/our-services/spinal-care/posterior-lumbar-decompression-discectomy
- https://spinesurgeons.ac.uk/Lumbar-Discectomy-and-Decompression
- https://www.newvictoria.co.uk/treatments/specialities-treatments/spinal-surgery/lumbar-discectomy
- https://pubmed.ncbi.nlm.nih.gov/23352565/
- https://www.ncbi.nlm.nih.gov/books/NBK544281/
- https://pubmed.ncbi.nlm.nih.gov/36328303/
- https://pubmed.ncbi.nlm.nih.gov/40434733/
- https://pubmed.ncbi.nlm.nih.gov/10586454/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC9421207/
- https://www.sciencedirect.com/science/article/abs/pii/S1529943018302419