Topics
Table of Contents

The human brain is a remarkable and intricate organ that governs all emotions, movements, and thoughts. Yet, because of ethical and technological constraints, direct brain research is extremely difficult. This is where brain organoids, also referred to as “mini-brains,” are useful. Brain organoid technology has developed quickly over the past ten years, providing researchers with a previously unheard-of window into human brain development, illness, and possible future therapies.
What brain organoids are, how they are created, their importance in neuroscience, and their potential in the future are all covered in this article.
Brain Organoids: What Are They?
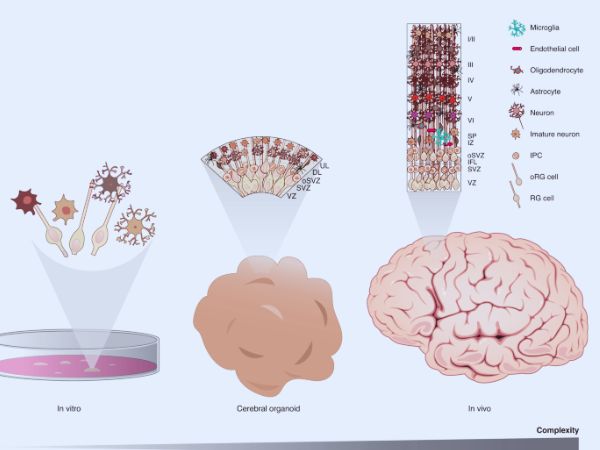
Brain organoids are miniature, three-dimensional, simplified representations of the human brain that are created in a lab using stem cells. These organoids can replicate some of the features and operations of the human brain despite their tiny size. They can mimic significant stages of development and disease processes, but they lack consciousness and complete brain function.
To put it simply, brain organoids are “models” of the brain that enable researchers to examine it in a petri dish.
How Do They Create Brain Organoids?
A number of intricate and intriguing steps are involved in the creation of brain organoids:
- The Initiation of stem cells
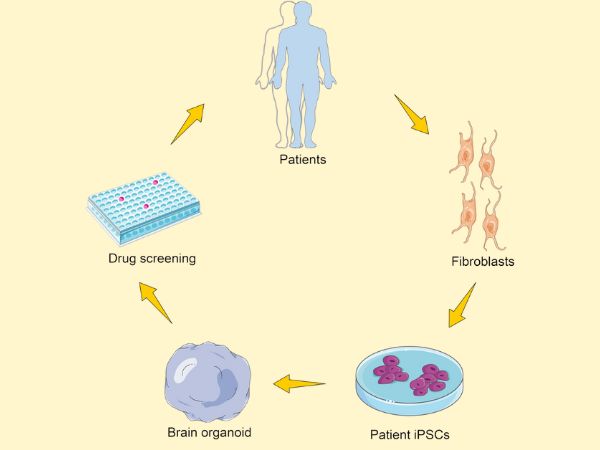
Either embryonic stem cells or induced pluripotent stem cells (iPSCs), which are adult cells that have been genetically altered to act like embryonic cells, are the starting point for everything.
- Induction of Neural
By providing these stem cells with particular growth factors and culture conditions, scientists can encourage them to develop into neural progenitor cells, which are the precursors of nervous tissue.
- 3D Culture
After that, these neural cells are put in bioreactors or unique gel-like matrices where they can self-organise into three-dimensional structures that mimic early-stage brain tissue.
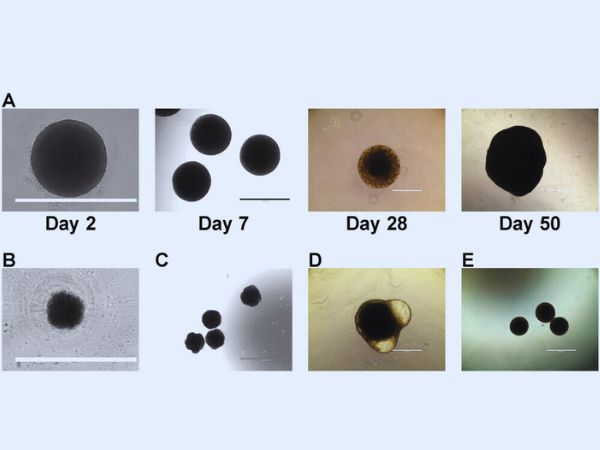
- Long-Term Development
These brain organoids generate different kinds of brain cells and build layers that resemble the cerebral cortex and other parts of the real human brain over the course of weeks to months.
What Do Brain Organoids Mimic?
Key characteristics of brain organoids can be replicated by:
- Early stages of brain development
- Development of the cortex, midbrain, and forebrain, three distinct brain regions
- Connections between neurones (synaptogenesis)
- Some pathological characteristics of illnesses like Alzheimer’s or microcephaly brought on by the Zika virus
They do not, however, have the intricate circuitry and blood supply (vascular system) of a fully formed human brain.
Uses for Brain Organoids

- Knowledge of Brain Development
Understanding how the human brain develops during the embryonic stage and what can go wrong in developmental disorders like autism or microcephaly is made easier by organoids.
- Researching Neurological Conditions
Researchers can conduct individualised studies of diseases like Parkinson’s, Alzheimer’s, epilepsy, and hereditary disorders by producing patient-specific organoids (from their own cells).
- Drug Discovery and Testing
Drug development is accelerated and the need for animal models is decreased by using brain organoids as platforms to assess the effects of novel medications on brain tissue.
- Infectious Disease Modelling
Organoids are still employed to research the effects of diseases like COVID-19 on the brain, and they were essential in the study of how the Zika virus causes birth abnormalities.
- Perspectives on Neurosurgery
Organoids are currently in the research stage, but by simulating drug reactions and illness mechanisms unique to each patient, they may one day direct surgical techniques.
Brain Organoids’ Drawbacks
Although brain organoids have the potential to be revolutionary, they have several drawbacks.
- Lack of Vascularization: Growth and lifespan are limited when there are no blood vessels to carry nutrients and oxygen.
- Incomplete Maturation: Compared to adult brains, organoids more closely resemble early foetal brain stages.
- Ethical Issues: As they grow more sophisticated, moral dilemmas about their application and possible consciousness surface.
- Variability: Varying lab procedures can produce uneven study outcomes.
Prospects for the Future
- Adding circulatory networks to organoids of the brain.
- Producing organoids that are more developed and useful.
- Organoids are being used in personalised medicine to forecast the course of diseases.
- Integrating artificial intelligence with brain organoids to further neurological research.
Brain organoids have the potential to revolutionise our knowledge of how the brain works, the treatment of neurological conditions, and neurosurgical procedures in the future.
In conclusion
One of the most fascinating areas of neuroscience is the creation of brain organoids. Organoids provide hope where conventional research techniques fail, from solving the enigmas surrounding brain development to discovering novel cures for debilitating illnesses. Even though we are just getting started, the advancements gained thus far point to a time when customised brain models may completely transform neurosurgery and neurological treatment.
Sources:
- https://pmc.ncbi.nlm.nih.gov/articles/PMC10420018/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC9726712/#s1
- https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2020.579659/full
- https://www.nature.com/articles/nature12517
- https://www.nature.com/articles/nature12517
- https://jbiomedsci.biomedcentral.com/articles/10.1186/s12929-021-00728-4
- https://www.hsci.harvard.edu/news/brain-organoids-replicate-key-events-human-brain-development
- https://journals.biologists.com/dev/article/146/8/dev166074/19861/Brain-organoids-advances-applications-and
- https://www.embs.org/pulse/articles/how-brain-organoids-are-revolutionizing-neuroscience/
- https://academic.oup.com/lifemedi/article/3/2/lnae014/7633788