Topics
Table of Contents
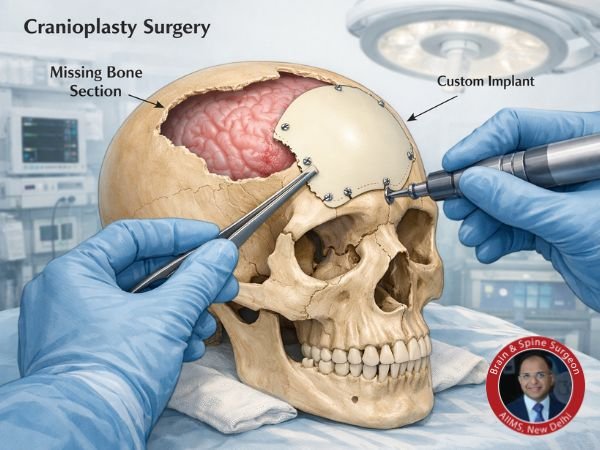
A neurosurgical operation called cranioplasty is used to fix a defect in the skull. It is typically done after a decompressive craniectomy, which is used to reduce brain swelling following a stroke, severe traumatic brain injury (TBI), or other serious diseases. Every patient and carer should be aware of the potential risks and consequences of cranioplasty, even though the treatment is frequently transformative, protecting the brain and restoring the integrity of the skull.
Comprehending Cranioplasty Surgery
Cranioplasty is a reconstructive surgical operation in which an implant composed of the patient’s own bone or a synthetic material like titanium or polymer replaces the missing section of the skull. It fulfils multiple functions:
Defence against external harm to the brain.
Improvement in some patients’ neurological function.
Restoration of the head’s physical shape and appearance.
Like all procedures, cranioplasty is usually considered safe, but it carries risks. Knowing these concerns can aid in prevention, early detection, and improved results.
Complications: Early vs. Late
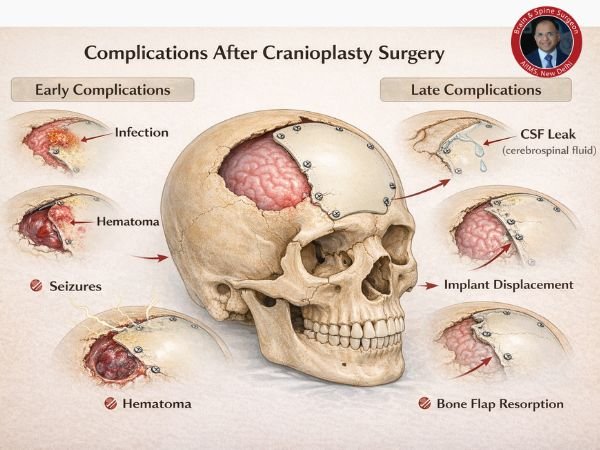
Early Issues
These happen in the days to weeks after surgery:
Infection of surgical wounds
Bleeding or the development of haematomas
Seizures
Cerebrospinal fluid (CSF) leak or swelling
Late Complications
Problems could show up months or years later:
Failure or displacement of implants
Resorption of bone flaps
Persistent infection
Deformities in appearance
According to research, the overall rate of complications following a cranioplasty might range from roughly 10% to nearly 40%, depending on the patient and the operative situation.
Implant Failure and Infection
One of the most frequent and important issues following cranioplasty is infection. It could happen near the implanted material or on the scalp incision. The following elements could raise this risk:

Previous wound infection history
Several surgeries
Reduced immunity
According to studies, infection rates for bacterial infections that are primarily associated with the bone flap or implant site in clinical cohorts usually fall between 5% and 12%.
Revision surgery and, in certain situations, a change to a more durable implant material may be necessary due to implant failure (e.g., displacement, resorption of bone).
Neurological Issues
In ways unrelated to the surgical wound, the brain itself may be affected:
Seizures may occur following surgery as a result of brain tissue inflammation.
Neurological deficiencies, either new or worsening (e.g., weakness, sensory alterations)
Hydrocephalus (fluid accumulation surrounding the brain) requires further care
Blood clot formation or stroke
Neurological function recovery frequently depends on the severity of the initial injury. For instance, based on clinical criteria including age and neurological exam scores, patients who sustain serious brain injury and remain in an unresponsive wakefulness or vegetative state may exhibit limited recovery, with just a tiny fraction regaining independence over time.
However, numerous studies have demonstrated that cranioplasty itself can enhance neurological status and functional outcomes, especially when done under ideal circumstances with careful surgical planning.
How Issues Are Handled
Early and efficient management is essential:
Antibiotics are used to treat infections, and in extreme situations, surgical cleaning or implant removal may be necessary.
Swelling or haematomas may require immediate surgical drainage.
Anti-seizure drugs and neurological assistance are used to control seizures.
Additional surgical correction may be necessary to treat CSF leaks.
In order to lower the risk of infection and other consequences, surgeons also take precautions during surgery, such as using rigorous sterile technique and handling tissues with care.
Monitoring Recovery
Phase of the Hospital
Usually, patients spend a few days in the hospital for:
Neurological surveillance
Care for wounds
Pain management
Following Discharge
The focus of follow-up appointments is:
Healing and assessment of scars
Evaluation of neurological function
Imaging to verify the location of the implant
It is advised to gradually resume regular activities in accordance with each person’s rehabilitation objectives.
In conclusion
Cranioplasty is an effective surgical technique for protection and perhaps neurological enhancement in addition to aesthetic skull rebuilding. However, being aware of the dangers and consequences associated with cranioplasty enables patients and their families to seek prompt care and make educated decisions. Most patients recover well and experience significant improvements in their quality of life with careful monitoring, careful follow-up, and appropriate surgical technique.
FAQs
1. What is the prognosis for a vegetative state following a brain injury?
When a patient appears awake but exhibits no symptoms of conscious awareness, they are said to be in a vegetative state. Long-term results vary greatly; prognosis is still difficult, and recovery towards independence is uncommon after three months, particularly in older persons.
2. Is neurological function always improved by cranioplasty?
Evidence indicates that many patients have neurological and functional benefits following cranioplasty, although this is not always the case. This is especially true when the procedure is performed at the right time, and there are no significant problems.
3. How long does it take to recover from a cranioplasty?
Depending on the patient’s health, the cause for the surgery, and any problems, a full recovery could take a few weeks to several months.
Sources:
- https://pubmed.ncbi.nlm.nih.gov/29533253/
- https://pubmed.ncbi.nlm.nih.gov/39315400/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC7184041/
- https://pubmed.ncbi.nlm.nih.gov/25827865/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC9533107/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC9665979/
- https://pubmed.ncbi.nlm.nih.gov/33686551/
- https://pubmed.ncbi.nlm.nih.gov/31953606/
- https://pubmed.ncbi.nlm.nih.gov/31082551/
- https://pubmed.ncbi.nlm.nih.gov/28823666/