Topics
Table of Contents
The complex anatomical area that connects the base of the skull to the upper cervical spine is known as the Craniovertebral Junction (CVJ). Significant mobility and stability are possible in this area, but it also contains vital neurological and circulatory systems, so any abnormality here would be extremely concerning from a clinical standpoint. If left untreated, congenital or acquired abnormalities in the CVJ might have severe neurological effects.
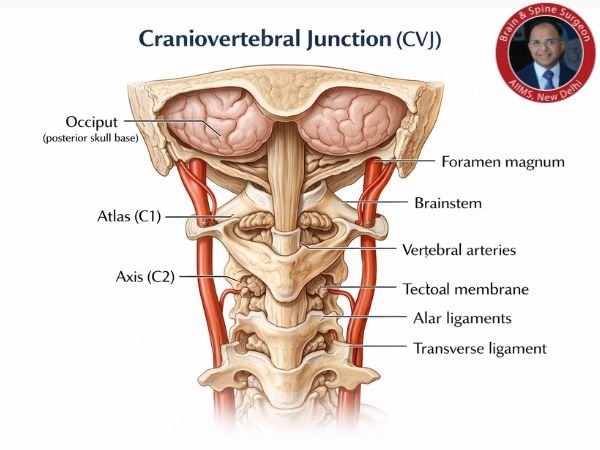
The craniovertebral (or craniocervical) junction (CVJ) is a collective term that refers to the occiput (Posterior skull base), atlas, axis and supporting ligaments. It is a transition zone between a mobile cranium & spinal column. It encloses the soft tissue structures of the cervicomedullary junction (medulla, spinal cord, and lower cranial nerves).
Related Post: Understanding Spinal Cord Injury and Its Surgical Management
We explore the management approaches, surgical procedures, applicable surgical anatomy, and complication avoidance that are pertinent to CVJ abnormalities in this blog.
CVJ Anomalies: What Are They?
A wide range of developmental or acquired disorders affecting the occipital bone, atlas (C1), axis (C2), and related ligaments and joints are referred to as CVJ abnormalities.
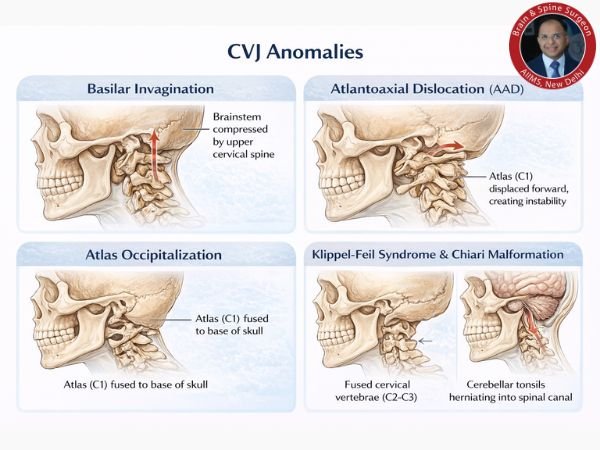
Typical CVJ abnormalities consist of:
Invagination of the basilar region
AAD, or atlantoaxial dislocation
Atlas occipitalization
Klippel-Feil illness
Chiari malformations, which are frequently linked to
These abnormalities may result from trauma, infection, or inflammatory diseases like rheumatoid arthritis, or they may be congenital or developmental.
Applied Anatomy in Surgery
It is essential to understand the surgical anatomy of the CVJ because of the following:
Upper Cervical Spinal Cord and Brainstem
Arteries of the vertebrae (going around C1–C2)
Nerves of the lower skull (IX–XII)
The Atlantoaxial and Atlanto-Occipital Joints
Stability is maintained by the transverse and alar ligaments.
Preoperative planning and intraoperative navigation are guided by precise understanding of neural pathways, vascular linkages, and bone landmarks, which lowers the chance of iatrogenic harm.
Symptoms of CVJ
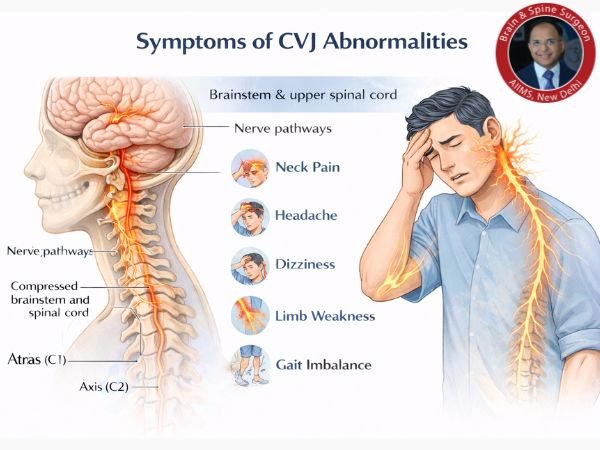
Headaches and back discomfort are typically the first signs of a craniocervical junction problem. When the head and neck are moved, as when coughing or bending forward, these symptoms usually get worse. Neck flexion in particular will make symptoms worse. One way to find out if the excessive mobility in this area is causing problems is to wear a hard cervical collar.
Spinal cord compression occurs in some of the most complicated upper cervical illnesses. Compression (squeezing or pressing) of the spinal cord can result in nerve-related issues that make day-to-day functioning difficult.
Identification / Diagnosis of Abnormalities in the Craniocervical Junction
Brain and upper spinal cord MRI or CT
Patients who experience neck or occiput pain together with neurologic abnormalities that can be attributed to the cerebellum, upper cervical spinal cord, or lower brain stem are suspected of having a craniocervical abnormality. Neuroimaging and clinical diagnosis (depending on the degree of spinal cord dysfunction) are typically used to differentiate illnesses of the lower cervical spine.
Neuroimaging
An MRI or CT scan of the brain and upper spinal cord, namely the posterior fossa and craniocervical junction, is performed if a craniocervical abnormalities is suspected. Deficits that are acute or abruptly worsening are emergencies that need to be imaged right away.
The best way to detect related soft-tissue lesions and neurological lesions (such as medulla, pons, cerebellum, spinal cord, and vascular abnormalities; syringomyelia) is with sagittal MRI. Compared to MRI, CT provides a more precise representation of bone structures and can be performed more quickly in an emergency.
In the absence of MRI and CT, x-rays are obtained, which include lateral views of the skull that reveal the cervical spine, anteroposterior views, and oblique views of the cervical spine.
CT myelography – CT following intrathecal injection of a radiopaque contrast agent—is performed if MRI is not available or is inconclusive and CT is also inconclusive. Vertebral angiography or magnetic resonance angiography is performed if MRI or CT indicates vascular problems.
Method of Management
1. Clinical Assessment
Symptoms include cranial nerve palsies, motor weakness, neck pain, increasing myelopathy, and abnormal gait.
Imaging: dynamic X-rays aid in evaluating instability; MRI and CT scans are crucial.
2. Surgical vs. Conservative
Conservative: Cervical collars, physical therapy, or careful monitoring may be used to treat mild, non-progressive instances.
Surgical: Recommended in cases of severe instability, deformity, or progressive neurological impairments.
Methods of Surgery
The disease and the anatomy of the patient determine the strategy. Among the methods frequently used are:
1. Techniques for Posterior Fixation
The Goel-Harms technique involves fixing the C1 lateral mass and the C2 pedicle/pars screw.
Occipitocervical Fusion (OCF): When C1 occipitalization occurs or instability spreads to the occiput.
Sublaminar rods and plates or wiring: In certain situations.
2. Endoscopic / Transoral Decompression
Recommended in cases of severe basilar invagination or irreducible ventral compression.
For stability, it can be used in conjunction with posterior fixation.
3. Fusion, Distraction, and Reduction
Posterior fusion after surgical reduction or gradual distraction using spacers.
4. Techniques That Are Not Too Invasive
Gaining traction as a result of decreased morbidity; calls for specific equipment and training.
Issues and How to Prevent Them
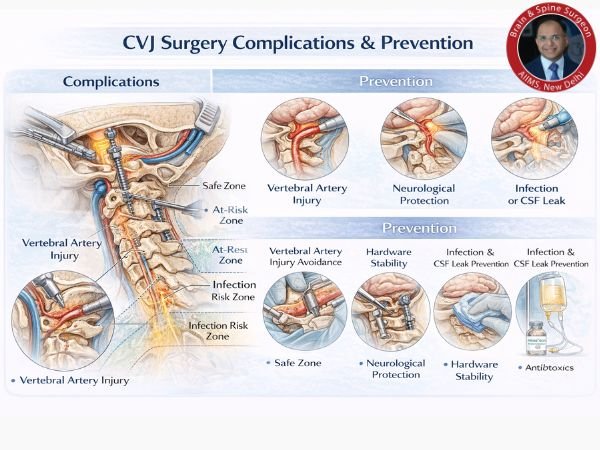
Vertebral Artery Injury Prevention: Careful dissection and screw trajectory planning; preoperative CT angiography to trace artery course.
Preventing Neurological Deficits: Cautious decompression, avoiding excessive traction, and intraoperative neuromonitoring (MEPs/SSEPs).
Hardware Failure / Non-union Prevention: Proper bone grafting, inflexible equipment, and patient adherence to immobilisation following surgery.
Infection / CSF Leak Avoidance: Strict asepsis, multilayer closure, and appropriate antibiotic prophylaxis.
Important Points
Abnormalities of the occipital bone, foramen magnum, or first two cervical vertebrae that reduce the space available for the lower brain stem and cervical cord are known as craniocervical junction abnormalities. These abnormalities can be congenital or acquired.
If a patient has neck or occiput pain together with neurologic abnormalities that can be attributed to the cerebellum, upper cervical spinal cord, or lower brain stem, you should suspect a craniocervical junction problem.
Use brain and upper spinal cord MRI or CT to identify craniocervical anomalies.
The squeezed neuronal structures should be reduced and rendered immobile.
Most patients should be treated with traction, immobilisation, or surgery if reduction doesn’t work.
In conclusion
Even though CVJ anomalies are complicated, they can be controlled with a methodical strategy based on precise anatomy, meticulous preparation, and skilled surgery. Patient outcomes have greatly improved as anatomical knowledge and surgical technology continue to progress.
Preventing irreversible brain damage in patients exhibiting symptoms of CVJ instability or deformity requires early diagnosis and specialised treatment.