Topics
Table of Contents
Glial cells in the brain or spinal cord are the source of gliomas, a form of tumor. The supporting cells of the nervous system, glial cells give neurones structure, defence, and nourishment. Roughly 80% of all malignant brain tumors and 30% of all brain tumors are gliomas.
The type of glial cell from which gliomas originate determines their classification:
- (from astrocytes) Astrocytomas
- (from oligodendrocytes) Oligodendrogliomas
- From ependymal cells, ependymomas
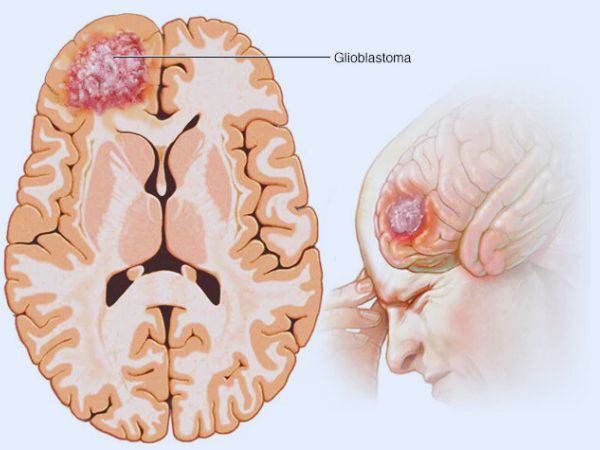
Furthermore, gliomas are categorised by the World Health Organisation (WHO) into four categories (I to IV) according to how aggressive they appear under a microscope. High-grade gliomas (Grades III and IV) grow more quickly and are more invasive than low-grade gliomas (Grades I and II), which grow more slowly. The most frequent and aggressive malignant primary brain tumor is glioblastoma multiforme (GBM), a Grade IV glioma.
Do gliomas come in different types?
Based on the kind of glial cell they originate in, gliomas can be divided into three primary categories. Multiple cell types can be found in certain gliomas. These are known as mixed gliomas by medical professionals. Based on their growth rate and other characteristics, they classify each form of glioma as low-, mid-, or high-grade.
Among the gliomas are:
- Glioblastomas and diffuse intrinsic pontine gliomas (DIPGs) are examples of astrocytes: Astrocytes are the cells that give rise to these tumors. Astrocytomas that grow quickly or are extremely aggressive are called glioblastomas. In adults, they are the most prevalent malignant brain tumor. Children frequently develop gliomas called astrocytes. DIPG is an uncommon but extremely aggressive kind of childhood brain cancer. It primarily affects children and develops in the brain stem.
- Ependymomas: These tumors originate in glial cells called ependymocytes. Ependymomas typically develop in the brain’s or spinal cord ventricles. They do not spread outside of the brain or spine, but they may do so through the cerebrospinal fluid, which envelops and shields the brain and spinal cord. About 2% of all brain tumors are ependymomas. Children are more likely than adults to have them.
- Oligodendrogliomas: These tumors begin as oligodendrocytes, which are glial cells. Although oligodendrogliomas typically grow more slowly, they have the potential to become more aggressive over time. They hardly ever spread outside of the brain or spine, just like ependymomas. Adults are more likely than children to have them. One to two percent of all brain tumors are oligodendrogliomas.
Glioma symptoms
The location, size, and growth rate of the tumor all affect the symptoms of gliomas. Typical signs and symptoms include:
- A headache
- Seizures
- Changes in personality or cognition
- Issues with memory
- Sensory abnormalities or motor weakness
- Visual disruptions
- Dizziness
- Weakness or numbness on one side of the body
- Difficulty in keeping balance and walking.
- Vomiting & Nausea
Who is susceptible to gliomas?
Gliomas can happen to anyone, but the following things could make you more susceptible:

- Age: Children under the age of twelve and older individuals over 65 are most likely to develop gliomas.
- Ethnicity: Compared to other races, white people may be more susceptible to gliomas.
- Family history: You may be more susceptible to gliomas if you have certain inherited genetic problems.
- Sex: Men are slightly more likely than women to get gliomas.
- Exposure to radiation or toxins: Prolonged or recurrent exposure to radiation or certain chemicals may raise your risk.
What is the frequency of gliomas?
In the United States, about 80,000 people receive a new primary brain tumor diagnosis every year. Gliomas make up about 25% of these.
Gliomas, especially those of the central nervous system (CNS), are seen in 5–10 out of every 100,000 people in India. About 2% of all malignant neoplasms in India are brain tumors, making up a sizable part of all brain tumors. Astrocytomas are a common kind of glioma, which can occur in both children and adults.
Why do gliomas occur or what is the cause?
According to research, gliomas and other brain and spinal cord tumors are caused by alterations in DNA. DNA is found in our genes. They guide cells on how to divide and multiply. Cells can proliferate uncontrollably if our genes’ DNA undergoes mutations.
Parents may pass on genetic mutations to you. They can also happen all at once while you’re alive.
What side effects might gliomas cause/complications?
The following are glioma complications that could be fatal:
- Bleeding in the brain, or brain haemorrhage.
- A brain herniation occurs when brain tissue shifts from its typical location within the skull.
- Hydrocephalus, or accumulation of fluid in the brain.
- Pressure within your head.
- Seizures.
How can gliomas be identified or diagnosed?
In addition to reviewing your medical history, your healthcare professional assesses your symptoms. A thorough neurological and physical examination will also be performed.
The most popular imaging tests for brain tumors are MRIs and CT scans. In addition to other tumors in your body, your doctor searches for brain tumors.
Doctor will perform a biopsy if your imaging scans reveal an abnormal lump. The process of analysing a tissue sample is called a biopsy. The biopsy will assist them in figuring out:
- If the growth is malignant.
- If an aberrant gene is the cause of the tumor.
- The tumor’s cell structure.
- The tumor’s grade, or aggressiveness.
Care and Therapy
How do you cure a glioma?
The following variables will affect your glioma treatment plan:
- If you have already had treatment for brain cancer.
- The tumor’s size, type, and location.
- Your age.
- Your well-being.
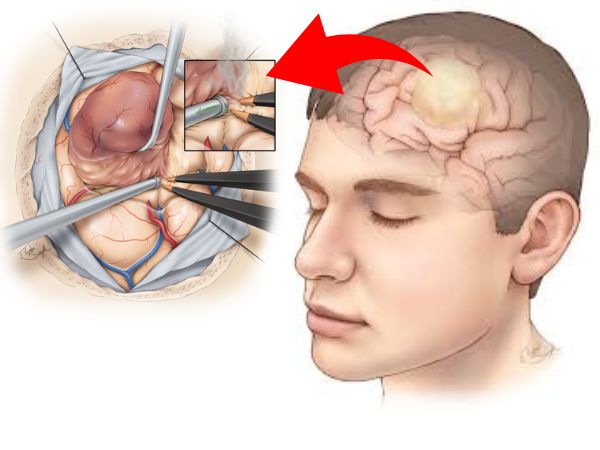
Surgery is typically the first course of treatment for gliomas. If the tumor is easily accessible, a surgeon might be able to remove it altogether. However, gliomas can be challenging to fully eradicate, particularly if they are in close proximity to sensitive brain regions or are difficult to reach.
Surgery should be followed by other therapies like radiation therapy and chemotherapy. These are adjuvant therapy, which means that following surgery, they eliminate any cancer cells or tumor components that may still be present. However, your doctor may employ radiation therapy or chemotherapy as your main therapies if a tumor cannot be removed.
Operation/Surgery
The most popular procedure for glioma removal is an open brain surgery called a craniotomy. You might be a candidate for laser ablation, depending on the tumor’s size and location. In this minimally invasive procedure, a brain tumor can be completely or partially destroyed using laser heat.
To guide the procedure, a surgeon may employ specialised methods like brain mapping or imaging. Brain mapping reveals the parts of your brain that regulate essential processes. By knowing this, your surgeon can prevent damaging or destroying vital brain tissue.
Radiation
Strong radiation doses are used in radiation therapy to eradicate tumors. For gliomas, your doctor might suggest radiation treatment. By precisely targeting the tumor’s form, radiation therapy reduces the possibility of harming nearby tissues.
Brachytherapy is another type of radiation treatment that you could get. To treat a tumor, a medical professional utilises radiation sources near the tumor. Radiation is released from the sources without damaging surrounding tissues.
Chemotherapy
Chemotherapy is the process of killing cancer cells with chemicals. It cures a variety of cancers. This treatment can be administered directly or orally.
One frequent chemotherapeutic medication used to increase the effectiveness of radiation therapy is temozolomide.
Avoidance/Prevention
How can gliomas be avoided?
The majority of glioma risk factors, including age and race, are uncontrollable. However, the evolution of low-grade gliomas into high-grade gliomas may be slowed or stopped by early detection and treatment. You might wish to think about genetic testing if brain tumors run in your family. Discuss the advantages and disadvantages of genetic testing with a genetic counsellor or your healthcare provider.
Additionally, it is wise to:
- Don’t expose your head to too much radiation.
- Keeping up a healthy way of living.
Prognosis and Outlook
What is the prognosis for glioma patients?
Glioma survival rates differ depending on the kind, grade, and age of the tumor. The prognosis may also be impacted by specific mutations. The prognosis is poorer for those who are diagnosed and treated later in life. Adults and children with low-grade ependymomas, oligodendrogliomas, and astrocytomas have the highest five-year survival rates. For glioblastomas, it is the lowest (between 6% and 20%).
Glioma Gamma Knife Radiosurgery
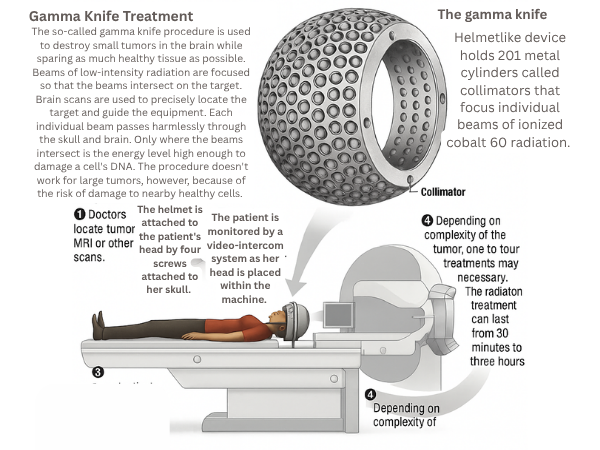
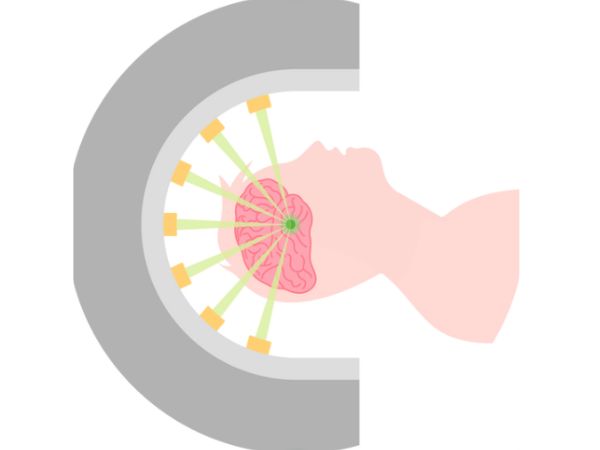
A type of stereotactic radiosurgery (SRS) called “gamma knife” uses intensely concentrated radiation beams to target the tumor while exposing the least amount of healthy brain tissue possible. It is especially helpful for gliomas that are in sensitive brain regions or are difficult to physically approach.
Radiosurgery with Gamma Knife for Low-Grade Gliomas
Gamma Knife radiosurgery provides a less invasive treatment option for low-grade gliomas (WHO Grade I and II) that can:
- After partial resection, control the growth of any remaining tumor.
- Treat well-defined, tiny lesions without requiring open surgery.
- Preserve neurocognitive function by delaying or minimising the need for whole-brain radiation.
Research has demonstrated that Gamma Knife can successfully treat low-grade gliomas with few adverse effects, providing long-lasting local control and enhanced quality of life. Younger patients or those with tumors in functionally sensitive areas benefit most from it.
Radiosurgery with Gamma Knife for High-Grade Gliomas
Treatment for high-grade gliomas, such as glioblastoma multiforme (GBM), is difficult and aggressive. Uses for Gamma Knife radiosurgery include:
- Recurrent High-Grade Gliomas: Used as a salvage treatment when tumors return following initial chemotherapy, radiation, and surgery.
- Targeting isolated or satellite lesions that are not responsive to additional surgical procedures is the goal of small residual or metastatic lesions.
In certain situations, Gamma Knife can effectively control tumors, extending survival and improving quality of life, however it should not be used in place of conventional treatment methods. To maximise results, multidisciplinary planning and careful patient selection are essential.
Gamma Knife Radiosurgery Benefits
- Precision: Accurately targets tumors within millimetres.
- Safety: Reduces the amount of radiation that reaches healthy brain tissue.
- Convenience: A short recovery period following an outpatient treatment.
- Repeatability: For recurrent tumors, it is possible to repeat if required.
In conclusion
Glioma treatment necessitates a customised, interdisciplinary strategy that strikes a balance between tumor control and neurological function preservation. A potent weapon in this arsenal is Gamma Knife radiosurgery, which gives patients with both low-grade and high-grade gliomas hope and better results.
For the best outcome, it is essential to speak with a skilled neurosurgeon who can explain the various treatment choices, including cutting-edge methods like Gamma Knife radiosurgery, if you or a loved one has been diagnosed with a glioma.
Sources:
- https://pmc.ncbi.nlm.nih.gov/articles/PMC4991137/
- https://www.ncbi.nlm.nih.gov/books/NBK441874/
- https://www.ncbi.nlm.nih.gov/books/NBK441874/#_article-18547_s13_
- https://my.clevelandclinic.org/health/diseases/21969-glioma
- https://www.mayoclinic.org/diseases-conditions/glioma/symptoms-causes/syc-20350251
- https://en.wikipedia.org/wiki/Glioma
- https://www.cancerresearchuk.org/about-cancer/brain-tumors/types/glioma-adults
- https://www.hopkinsmedicine.org/health/conditions-and-diseases/gliomas
- https://www.cancer.gov/publications/dictionaries/cancer-terms/def/glioma
- https://braintumorresearch.org/pages/types-of-brain-tumors-glioma?srsltid=AfmBOoqH0Fueb1M3QbNjKjiS2AYdxR-3CORqtBkctpVf9LrxEQ9I_Hzy
You May Also Know Related to Gamma Knife
FAQ’s
How does Gamma Knife work?
Gamma Knife uses 192–201 precisely focused beams of gamma rays that converge at a single target point in the brain. This high dose of radiation damages the DNA of abnormal cells, stopping their growth or causing them to shrink, while minimizing exposure to nearby healthy tissue.
Is Gamma Knife a surgery?
No, Gamma Knife is not a traditional surgery. It is a non-invasive outpatient procedure performed without any incision, stitches, or general anesthesia in most cases.
What conditions can be treated with Gamma Knife?
Gamma Knife is commonly used for:
Brain tumors (benign and malignant)
Metastatic brain lesions
Arteriovenous malformations (AVMs)
Trigeminal neuralgia
Acoustic neuromas (vestibular schwannomas)
Pituitary tumors
Certain functional disorders (like tremors)
Is Gamma Knife painful?
The procedure is generally painless. Patients may feel mild pressure while the head frame (if used) is applied or may experience slight discomfort from anesthesia injections, but the treatment itself is not painful.
How long does the procedure take?
Depending on the condition and treatment plan, Gamma Knife may take 30 minutes to 3 hours. Most patients go home the same day.
What are the possible side effects?
Common side effects are usually mild and temporary, including:
Headache
Nausea
Fatigue
Mild scalp swelling or tenderness at the frame site
Rarely, some patients may experience delayed radiation effects such as brain swelling or radiation necrosis.
When can the patient return to normal activities after Gamma Knife?
Most patients can return to their normal routine within 24–48 hours after the procedure.
You may feel mild fatigue for a few days.
Follow-up imaging is usually required after 1 year.
How effective is Gamma Knife?
Gamma Knife has a high success rate and has been used worldwide for decades. Its effectiveness depends on the condition treated, size and location of the lesion, and overall patient health. In many cases, it offers results comparable to open surgery with fewer risks.
Can Gamma Knife be repeated if needed?
Yes, in some cases Gamma Knife treatment can be repeated if the disease recurs or if new lesions develop.
Is Gamma Knife safe?
Yes. Gamma Knife is considered one of the safest and most precise forms of radiosurgery, with millions of patients treated globally and extensive clinical data supporting its use.
Who is eligible for Gamma Knife treatment?
Eligibility depends on factors such as:
Size and location of the lesion
Overall health and age
Whether open surgery is too risky
A neurosurgeon and radiation oncologist will decide if Gamma Knife is the best option for you.
What happens before the procedure?
A detailed MRI or CT scan is performed to map the brain.
A lightweight head frame or mask is used for accuracy.
Your doctors plan the radiation dose and target areas using specialized software.
Will I need anesthesia?
Local anesthesia is given if a head frame is used.
General anesthesia is usually not required, except for children or patients unable to remain still.
What is the cost of Gamma Knife in India?
Costs vary depending on hospital, city, and condition treated. On average, Gamma Knife in India ranges from ₹1.5 lakh to ₹4.5 lakh. It is usually more affordable compared to treatment in Western countries. At AIIMS Delhi, it is much more affordable around ₹75,000 which makes it affordable for the patients in need.
Where can I get Gamma Knife treatment in Delhi?
AIIMS Delhi is one of the leading centres for Gamma Knife in India.
AIIMS uses the latest Gamma Knife Perfexion system.
It has successfully treated thousands of patients for brain tumors, blood vessel problems, and even eye cancers.
The treatment is done by expert neurosurgeons such as Dr. Deepak Agrawal and team.
Clinic timings for Gamma Knife OPD at AIIMS Delhi: Monday & Friday, 8:00 AM – 9:00 AM.
Cost is around ₹75,000 and is subsidized compared to private hospitals.
What is the complete process of the Gamma Knife?
The whole procedure is usually done in one day:
- Consultation & Planning – Doctors review your scans and decide the treatment.
- Head Frame/Mask – A lightweight frame or mask is placed to keep your head still.
- Imaging – MRI/CT scans are done to locate the exact target.
- Treatment Planning – Specialists plan the dose and direction of radiation.
- Gamma Knife Treatment – You lie on the machine; painless radiation beams treat the target (30 mins–3 hrs).
- Recovery & Discharge – The frame is removed, and most patients go home the same day.
- Follow-up – MRI after a few months to check results.
What formalities do I have to complete prior to getting the date of GK?
Before you get a treatment date, you need to complete a few steps:
- OPD Registration – Visit the Neurosurgery OPD (Gamma Knife clinic at AIIMS, Mon & Fri 8–9 AM) and register.
- Consultation with Doctor – Meet the neurosurgeon who will check your reports, MRI/CT scans, and medical history.
- Investigations – Sometimes fresh MRI/CT or blood tests are needed for treatment planning.
- Medical Fitness – Basic checks like blood pressure, sugar, heart condition, etc.
Financial/Insurance Approval –
- If using Ayushman Bharat or government schemes, you need approval papers.
- If self-paying, you will be given the estimated cost (~₹75,000 at AIIMS).
- Consent & Admission Slip – Once doctors confirm you are fit and formalities are done, you sign the consent form.
- Treatment Date Allotment – A date is given for your Gamma Knife procedure.
What formalities do I have to complete after getting the date of GK?
Once you receive your Gamma Knife date, you’ll need to do a few simple things before the procedure:
- Admission Process – Report to AIIMS on the morning of your procedure and complete admission at the Neurosurgery ward/Daycare.
- Paperwork – Carry your OPD slip, MRI/CT films, blood test reports, admission slip, and ID proof. If you are covered under Ayushman Bharat/insurance, keep those approval papers ready.
- Consent Forms – You (or a family member) will sign consent for the procedure and anesthesia.
- Medical Check-up – Doctors will check your BP, sugar, heart rate, and do a quick physical exam.
- Fasting – Usually, you will be asked to not eat or drink for 6 hours before the procedure.
- Pre-Procedure Prep – An IV line may be put, and medicines (sedation/antibiotics if needed) are given.
- Treatment – You are then taken to the Gamma Knife room for frame/mask placement, imaging, and treatment.
After the procedure, you’ll be observed for a few hours and most patients are discharged the same day or next morning.
What investigations to be done?
Urea & creatinine
Should I come fasting?
No, You can have light breakfast.
In case of HT/DM should take my medicines?
Yes, you can take the medicine and then come for the treatment.