Topics
Table of Contents
Hurler syndrome, also known as mucopolysaccharidosis type I (MPS I), is a rare genetic disorder that affects the body’s ability to break down certain types of sugar molecules called glycosaminoglycans (GAGs). This condition belongs to a group of disorders called mucopolysaccharidoses, which result from the deficiency of enzymes necessary for the breakdown of GAGs. Hurler syndrome specifically involves a deficiency of the enzyme alpha-L-iduronidase.
Types of Hurler Syndrome
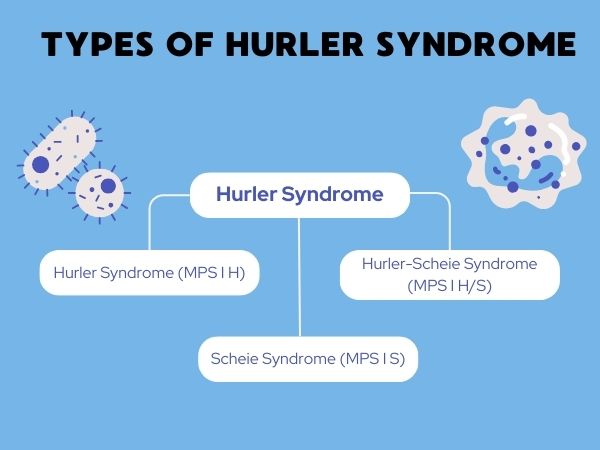
Hurler syndrome can be classified into three subtypes based on the severity of symptoms:
- Hurler Syndrome (MPS I H): This is the most severe form of MPS I, characterized by early onset and rapid progression of symptoms.
- Hurler-Scheie Syndrome (MPS I H/S): This form is intermediate in severity, with symptoms appearing later in childhood and progressing more slowly than in MPS I H.
- Scheie Syndrome (MPS I S): This is the mildest form of MPS I, with symptoms typically appearing later in childhood and progressing slowly. Individuals with Scheie syndrome usually have a normal lifespan.
Signs and Symptoms

The signs and symptoms of Hurler syndrome can vary widely but often include:
- Coarse facial features
- Enlarged liver and spleen (hepatosplenomegaly)
- Corneal clouding
- Joint stiffness and contractures
- Skeletal abnormalities
- Heart disease
- Respiratory problems
- Hearing loss
- Developmental delay
- Intellectual disability
Causes of Hurler Syndrome

Hurler syndrome is caused by mutations in the IDUA gene, which provides instructions for making the alpha-L-iduronidase enzyme. Without this enzyme, the body cannot break down certain GAGs, leading to their accumulation in cells and tissues throughout the body. This buildup causes progressive damage and dysfunction in various organs and systems.
Prevention
Since Hurler syndrome is a genetic disorder, it cannot be prevented. However, genetic counseling and prenatal testing can help identify individuals at risk of passing on the condition to their children.
Diagnosis
Diagnosing Hurler disease typically involves a combination of clinical evaluation, imaging studies, enzyme assays, and genetic testing. Clinical features such as facial appearance, skeletal abnormalities, and organ enlargement may raise suspicion for MPS I, prompting further diagnostic testing.
Treatment of Hurler Syndrome

While there is currently no cure for Hurler syndrome, various treatment approaches can help manage symptoms and improve quality of life:
- Enzyme Replacement Therapy (ERT): ERT involves intravenous infusion of a synthetic form of the missing enzyme, alpha-L-iduronidase. This therapy aims to replace the deficient enzyme and reduce the buildup of GAGs in the body.
- Hematopoietic Stem Cell Transplantation (HSCT): HSCT, also known as bone marrow transplant, can be used to replace defective cells with healthy ones capable of producing the missing enzyme. Early transplantation, ideally before the onset of irreversible organ damage, offers the best chance for successful outcomes.
- Symptomatic Management: Various medications and therapies may be used to manage specific symptoms associated with Hurler’s disease, such as pain management, physical therapy, and hearing aids.
Home Remedies and Supportive Care

While there are no specific home remedies for Hurler disease, supportive care, and lifestyle modifications can help improve the quality of life for individuals with this condition. This may include:
- Regular medical follow-ups to monitor disease progression and manage complications
- Physical and occupational therapy to improve mobility and function
- Assistive devices and adaptive equipment to support daily activities
- Nutritional support to address feeding difficulties and ensure adequate calorie intake
- Emotional and psychological support for patients and their families, including access to support groups and counseling services
In conclusion, Hurler syndrome is a rare and debilitating genetic disorder that affects multiple organs and systems in the body. While there is currently no cure, advances in medical management have significantly improved the prognosis and quality of life for individuals with this condition. Early diagnosis, comprehensive medical care, and ongoing support are essential components of managing Hurler syndrome and optimizing outcomes for affected individuals and their families.