Topics
Table of Contents

Treatment for brain disorders has changed as a result of advances in neurosurgery. Minimally Invasive Brain Surgery (MIBS), a cutting-edge surgical technique that enables neurosurgeons to treat complicated brain problems with fewer incisions, more accuracy, and quicker recovery, is one of the most important innovations.
In order to help patients and their families make confident decisions, this page discusses what minimally invasive brain surgery is, who requires it, its advantages, risks, recovery process, and commonly asked questions.
Minimally Invasive Brain Surgery: What Is It?
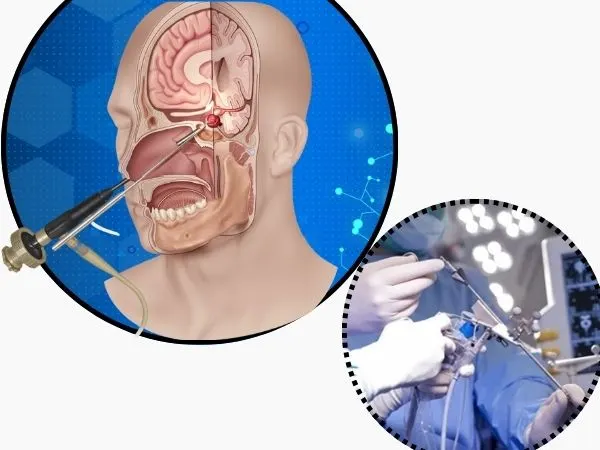
Instead of using huge skull incisions (craniotomies) to treat brain diseases, minimally invasive brain surgery uses tiny openings, sophisticated imaging, microscopes, endoscopes, and navigation systems.

The objective is to:
Get to the impacted area securely
Prevent harm to healthy brain tissue
Minimise discomfort, blood loss, and hospital stays
This method achieves better results with less brain damage by combining technology and surgical skill.
Conditions Addressed by Minimally Invasive Brain Surgery
The following conditions can be treated with minimally invasive methods:
Brain tumours, both benign and some malignant
Tumours of the pituitary
Hydrocephalus (blockage of the CSF)
Brain bleeding, or intracerebral haemorrhage
Vascular abnormalities and aneurysms
Neuralgia trigeminal
Surgery for epilepsy (selected cases)
Brain cysts
Brain compression associated with the spine
Minimally invasive surgery is not appropriate for all patients. Tumour size, location, patient health, and neurological state all play a role in the decision.
Minimally Invasive Brain Surgery Types

1. Endoscopic Brain Surgery
Uses a tiny incision or natural holes, such as the nose, to introduce a thin camera (endoscope) (endoscopic skull base surgery).
2. Craniotomy using a keyhole
A tiny hole in the skull through which tiny equipment and microscopes are used to do surgery.
3. Guided Surgery using Neuro-Navigation
The surgeon is extremely accurately guided by GPS-like imaging equipment.
4. Stereotactic Procedures
Extremely accurate targeting for deep brain operations or biopsies.
5. Haematoma Evacuation with Minimal Invasiveness
Used to remove brain clots with the least amount of tissue damage possible.
Advantages of Brain Surgery with Minimal Invasion
MIBS has a number of benefits over conventional open brain surgery, including:
Less scars and a smaller incision
Reduced harm to healthy brain tissue
Decreased haemorrhage
Reduced chance of infection
Reduced discomfort following surgery
A shorter hospital stay
Quicker recuperation and resumption of regular activities
Improved cosmetic results
Potential Dangers and Issues
No brain surgery is totally risk-free, even if minimally invasive procedures are safer. Potential dangers consist of:
Bleeding
An infection
Neurological impairments, either temporary or permanent
Leak of CSF
Seizures
Incomplete tumour removal (in some situations)
Rarely, conversion to open surgery is required
Before proposing surgery, a skilled neurosurgeon carefully weighs the advantages and disadvantages.
What to anticipate before to surgery
Prior to surgery, patients typically go through:

CT or MRI scan
Heart assessment and blood tests
Neurological assessment
Evaluation of anaesthesia
Comprehensive patient and family counselling
The surgeon clarifies:
Why surgery is necessary
The kind of planned operation
Anticipated result
Potential dangers and options
What Takes Place During Surgery?

General anaesthesia is used during surgery.
The surgeon is guided by advanced imaging and navigation.
Through tiny apertures, specialised equipment are utilised.
The length of surgery varies on the ailment.
The preservation of brain function and patient safety continue to be of utmost importance.
Rehabilitation Following Minimally Invasive Brain Surgery
Hospitalisation
Depending on the operation, the majority of patients are released in two to five days.
Pain and Recovery
Usually, pain is minimal and effectively managed with medication.
Smaller wounds heal more quickly.
Go Back to Your Ordinary Life
Light exercises: one to two weeks
Work: 2–6 weeks, depending on the type of surgery
Each patient experiences a different level of full healing.
Follow-up
To track recovery, imaging and routine follow-ups could be necessary.
What Makes a Perfect Candidate?
You might qualify if:
There is a minimally invasive way to access the lesion.
It doesn’t require a lot of brain exposure.
You are in good enough health to have surgery.
Expert neurosurgical review determines final appropriateness.
Professional Care Is Important
High surgical skill, sophisticated equipment, and careful preparation are necessary for minimally invasive brain surgery. Patients can anticipate safer surgeries, better results, and a quicker recovery when under the care of a skilled neurosurgeon.
A thorough consultation can help evaluate whether a minimally invasive method is appropriate if brain surgery has been recommended for you or your loved one.
FAQ’s
1. Is it safe to perform minimally invasive brain surgery?
Indeed. It is regarded as safe and effective for some disorders when carried out by a skilled neurosurgeon utilising cutting-edge equipment.
2. Will you shave my hair?
In contrast to typical surgery, that needs extensive shaving, only a tiny region may be shaved.
3. Compared to open brain surgery, is it less painful?
Indeed. Less pain and a speedier recovery are associated with smaller incisions.
4. What is the duration of the procedure?
Depending on how complicated the issue is, it can take anywhere from one to six hours.
5. After surgery, will I require rehabilitation?
Depending on neurological involvement, some patients may require occupational therapy, speech therapy, or physiotherapy.
6. Can all brain tumours be treated with minimally invasive surgery?
No. Open surgery is still necessary for certain tumours. The choice is personal.
7. What is the percentage of success?
Minimally invasive methods typically provide good results with fewer consequences, while success varies depending on the condition being treated.
8. After surgery, when should I get in touch with the doctor?
Right away if there is:
An intense headache
A fever
Growing weakness
Seizures
leakage from the injury
9. Is it possible to repeat minimally invasive brain surgery if necessary?
Indeed. In certain situations, minimally invasive procedures can be safely repeated if the illness recurs or needs more care. The choice is based on the type of brain problem, the patient’s recuperation, and general health.
10. Is the cost of minimally invasive brain surgery higher than that of conventional surgery?
Even though using cutting-edge technology may result in higher initial costs, the overall cost is frequently offset by shorter hospital stays, fewer complications, quicker healing, and a decreased need for long-term medication or therapy, making it cost-effective over time.
Sources
https://arogyajivan.com/neurology/blog/minimally-invasive-brain-tumor-surgery-india-benefits-risks
https://www.jaslokhospital.net/blogs/benefits-of-minimally-invasive-neurosurgery-you-must-know
https://drninadpatil.com/minimally-invasive-neurosurgery-benefits-risks-and-what-to-expect/
https://my.clevelandclinic.org/health/treatments/16802-brain-surgery
https://www.parkview.com/blog/the-pros-and-cons-of-minimally-invasive-brain-surgery