Topics
Table of Contents
Parasagittal and Parafalcine Meningiomas: What Are They?
Tumors known as meningiomas develop from the meninges, which are the protective coverings that envelop the brain and spinal cord. Although the majority of meningiomas are benign, the pressure they place on other brain structures can result in serious issues.
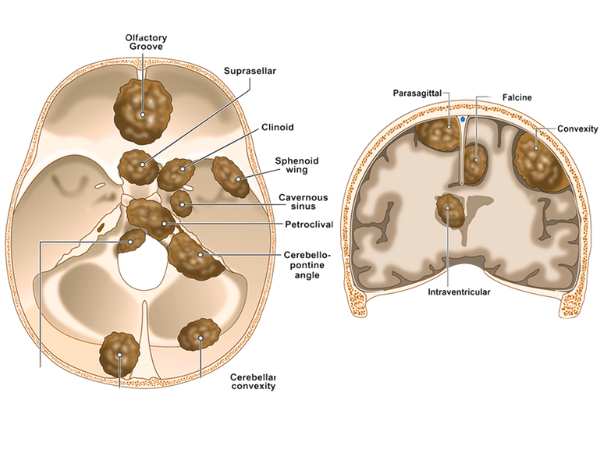
Two major forms of meningiomas that develop along the brain’s midline are parasagittal and parafalcine:
- Parasagittal Meningiomas: Develop close to the major vein that runs along the top of the brain, the superior sagittal sinus.
- The parafalcine The falx cerebri, a sickle-shaped fold of dura mater that divides the two cerebral hemispheres, is where meningiomas form.
Because of their position, these Tumors may induce symptoms even when they develop slowly, particularly if they compress vital brain regions or venous sinuses.
Reasons & Risks
Meningiomas are linked to a number of risk factors, while their exact cause is unknown:
- Genetic susceptibility (e.g., type 2 neurofibromatosis)
- Exposure to radiation
- More prevalent in women, hormonal impacts
- Usually diagnosed between the ages of 40 and 70
Parasagittal/Parafalcine Meningioma Symptoms
The tumor’s location and size affect the symptoms. These Tumors frequently impact the motor and sensory parts of the legs because they develop close to the midline of the brain. Typical signs and symptoms include:
- One or both legs feeling weak or numb
- Seizures
- Headache
- Changes in cognition or personality
- Abdominal control loss (in big Tumors)
- Indications of elevated intracranial pressure (when there is brain swelling or sinus compression)
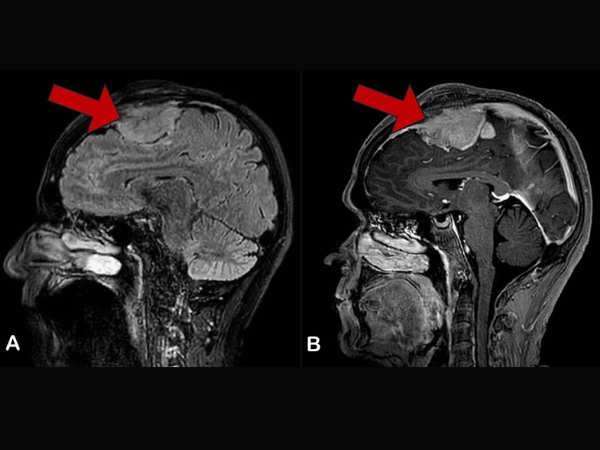
Diagnosis
A thorough diagnosis consists of:
- The gold standard for identifying and describing meningiomas is MRI with contrast.
- A CT scan can be useful in detecting any calcifications or involvement of the bones.
- MR Venography: Crucial for assessing the superior sagittal sinus’s involvement
- To confirm the diagnosis and classify the Tumor as benign, atypical, or malignant, a biopsy may be required.
Options for Treatment
Tumor size, location, growth rate, and symptoms all impact treatment options:
- Observation
Regular imaging follow-up may be advised for older patients with tiny, asymptomatic Tumors.
- Excision via Surgery
The primary treatment for accessible Tumors that are producing symptoms is surgery. However, because parasagittal/parafalcine meningiomas are close to important blood arteries like the superior sagittal sinus, they can be difficult to fully remove.
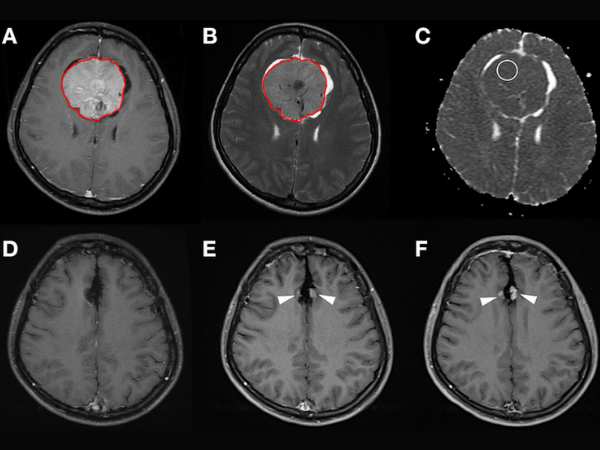
- Radiosurgery Using Gamma Knife
This is a very successful non-invasive procedure that can be utilised either:
- As the main course of treatment for minor Tumors
- Targeting any remaining Tumors after surgery
- Regarding recurring Tumors
Radiosurgery with Gamma Knife for Parasagittal/Parafalcine Meningiomas
Gamma Knife Benefits for These Tumors:

- Non-invasive; no anaesthesia or incision is necessary
- Quick recovery from an outpatient procedure
- Perfect for Tumors that are close to important structures (such as the superior sagittal sinus).
- Low rates of complications
- Elevated rates of Tumor control (>90% in benign meningiomas)
A Candidate Is Who?
- Individuals with Tumors that are small to larger in size
- Tumors near or involving the venous sinuses, where there is a greater risk of surgery
- Patients who are not surgically fit
- Recurring Tumors following previous operations
Overview of the Procedure:
- Planning based on MRI
- For accuracy, a lightweight frame or frameless mask is utilised.
- Usually, one session is enough to finish the treatment.
- On the same day, patients go home.
Prognosis and Follow-Up
The long-term results of parasagittal/parafalcine meningiomas are quite good when they are treated with surgery, Gamma Knife, or both. To check for Tumor control or recurrence, routine MRI scans are required.
In conclusion
Despite usually being benign, parasagittal and parafalcine meningiomas can have a major effect on neurological function because of where they are located. Excellent results with little risk can be achieved with early diagnosis and customised treatment, which frequently combines microsurgery and Gamma Knife Resonance Imaging.
Source:
- https://pmc.ncbi.nlm.nih.gov/articles/PMC6889965/
- https://www.sciencedirect.com/science/article/abs/pii/B9780128221983000318
- https://www.healthline.com/health/brain-tumor/parafalcine-meningioma
- https://www.tandfonline.com/doi/full/10.1080/02688697.2019.1635988?scroll=top&needAccess=true
- https://www.sciencedirect.com/science/article/abs/pii/S1878875018329401
- https://www.medicalnewstoday.com/articles/parasagittal-meningioma#diagnosis
- https://pubmed.ncbi.nlm.nih.gov/26115473/
- https://pubmed.ncbi.nlm.nih.gov/23930861/
- https://www.redjournal.org/article/S0360-3016(09)01590-9/fulltext
You May Also Know Related to Gamma Knife
FAQ’s
How does Gamma Knife work?
Gamma Knife uses 192–201 precisely focused beams of gamma rays that converge at a single target point in the brain. This high dose of radiation damages the DNA of abnormal cells, stopping their growth or causing them to shrink, while minimizing exposure to nearby healthy tissue.
Is Gamma Knife a surgery?
No, Gamma Knife is not a traditional surgery. It is a non-invasive outpatient procedure performed without any incision, stitches, or general anesthesia in most cases.
What conditions can be treated with Gamma Knife?
Gamma Knife is commonly used for:
Brain tumors (benign and malignant)
Metastatic brain lesions
Arteriovenous malformations (AVMs)
Trigeminal neuralgia
Acoustic neuromas (vestibular schwannomas)
Pituitary tumors
Certain functional disorders (like tremors)
Is Gamma Knife painful?
The procedure is generally painless. Patients may feel mild pressure while the head frame (if used) is applied or may experience slight discomfort from anesthesia injections, but the treatment itself is not painful.
How long does the procedure take?
Depending on the condition and treatment plan, Gamma Knife may take 30 minutes to 3 hours. Most patients go home the same day.
What are the possible side effects?
Common side effects are usually mild and temporary, including:
Headache
Nausea
Fatigue
Mild scalp swelling or tenderness at the frame site
Rarely, some patients may experience delayed radiation effects such as brain swelling or radiation necrosis.
When can the patient return to normal activities after Gamma Knife?
Most patients can return to their normal routine within 24–48 hours after the procedure.
You may feel mild fatigue for a few days.
Follow-up imaging is usually required after 1 year.
How effective is Gamma Knife?
Gamma Knife has a high success rate and has been used worldwide for decades. Its effectiveness depends on the condition treated, size and location of the lesion, and overall patient health. In many cases, it offers results comparable to open surgery with fewer risks.
Can Gamma Knife be repeated if needed?
Yes, in some cases Gamma Knife treatment can be repeated if the disease recurs or if new lesions develop.
Is Gamma Knife safe?
Yes. Gamma Knife is considered one of the safest and most precise forms of radiosurgery, with millions of patients treated globally and extensive clinical data supporting its use.
Who is eligible for Gamma Knife treatment?
Eligibility depends on factors such as:
Size and location of the lesion
Overall health and age
Whether open surgery is too risky
A neurosurgeon and radiation oncologist will decide if Gamma Knife is the best option for you.
What happens before the procedure?
A detailed MRI or CT scan is performed to map the brain.
A lightweight head frame or mask is used for accuracy.
Your doctors plan the radiation dose and target areas using specialized software.
Will I need anesthesia?
Local anesthesia is given if a head frame is used.
General anesthesia is usually not required, except for children or patients unable to remain still.
What is the cost of Gamma Knife in India?
Costs vary depending on hospital, city, and condition treated. On average, Gamma Knife in India ranges from ₹1.5 lakh to ₹4.5 lakh. It is usually more affordable compared to treatment in Western countries. At AIIMS Delhi, it is much more affordable around ₹75,000 which makes it affordable for the patients in need.
Where can I get Gamma Knife treatment in Delhi?
AIIMS Delhi is one of the leading centres for Gamma Knife in India.
AIIMS uses the latest Gamma Knife Perfexion system.
It has successfully treated thousands of patients for brain tumors, blood vessel problems, and even eye cancers.
The treatment is done by expert neurosurgeons such as Dr. Deepak Agrawal and team.
Clinic timings for Gamma Knife OPD at AIIMS Delhi: Monday & Friday, 8:00 AM – 9:00 AM.
Cost is around ₹75,000 and is subsidized compared to private hospitals.
What is the complete process of the Gamma Knife?
The whole procedure is usually done in one day:
- Consultation & Planning – Doctors review your scans and decide the treatment.
- Head Frame/Mask – A lightweight frame or mask is placed to keep your head still.
- Imaging – MRI/CT scans are done to locate the exact target.
- Treatment Planning – Specialists plan the dose and direction of radiation.
- Gamma Knife Treatment – You lie on the machine; painless radiation beams treat the target (30 mins–3 hrs).
- Recovery & Discharge – The frame is removed, and most patients go home the same day.
- Follow-up – MRI after a few months to check results.
What formalities do I have to complete prior to getting the date of GK?
Before you get a treatment date, you need to complete a few steps:
- OPD Registration – Visit the Neurosurgery OPD (Gamma Knife clinic at AIIMS, Mon & Fri 8–9 AM) and register.
- Consultation with Doctor – Meet the neurosurgeon who will check your reports, MRI/CT scans, and medical history.
- Investigations – Sometimes fresh MRI/CT or blood tests are needed for treatment planning.
- Medical Fitness – Basic checks like blood pressure, sugar, heart condition, etc.
Financial/Insurance Approval –
- If using Ayushman Bharat or government schemes, you need approval papers.
- If self-paying, you will be given the estimated cost (~₹75,000 at AIIMS).
- Consent & Admission Slip – Once doctors confirm you are fit and formalities are done, you sign the consent form.
- Treatment Date Allotment – A date is given for your Gamma Knife procedure.
What formalities do I have to complete after getting the date of GK?
Once you receive your Gamma Knife date, you’ll need to do a few simple things before the procedure:
- Admission Process – Report to AIIMS on the morning of your procedure and complete admission at the Neurosurgery ward/Daycare.
- Paperwork – Carry your OPD slip, MRI/CT films, blood test reports, admission slip, and ID proof. If you are covered under Ayushman Bharat/insurance, keep those approval papers ready.
- Consent Forms – You (or a family member) will sign consent for the procedure and anesthesia.
- Medical Check-up – Doctors will check your BP, sugar, heart rate, and do a quick physical exam.
- Fasting – Usually, you will be asked to not eat or drink for 6 hours before the procedure.
- Pre-Procedure Prep – An IV line may be put, and medicines (sedation/antibiotics if needed) are given.
- Treatment – You are then taken to the Gamma Knife room for frame/mask placement, imaging, and treatment.
After the procedure, you’ll be observed for a few hours and most patients are discharged the same day or next morning.
What investigations to be done?
Urea & creatinine
Should I come fasting?
No, You can have light breakfast.
In case of HT/DM should take my medicines?
Yes, you can take the medicine and then come for the treatment.