Topics
Table of Contents
Despite its small size, the pineal area of the brain is crucial to neurological function. It can be difficult to diagnose and cure Tumors that develop in this deeply ingrained area. Treatment results have greatly improved with the introduction of sophisticated neurosurgery procedures such as Gamma Knife radiosurgery. A comprehensive explanation of pineal area Tumors, including their symptoms, diagnosis, available treatments, and the function of Gamma Knife therapy, is the goal of this article.

The Pineal Region: What is it?
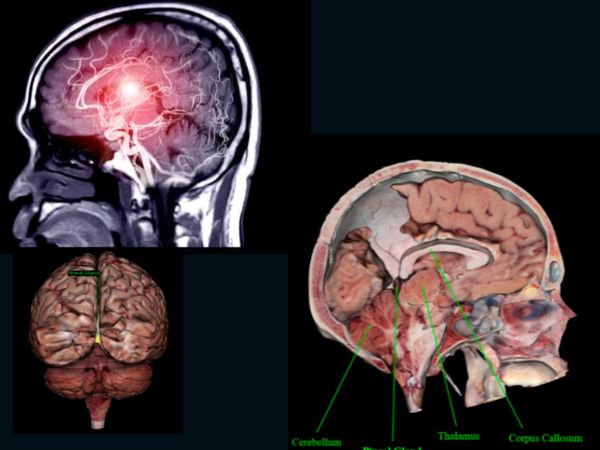
The pineal area is situated behind the third ventricle, just above the cerebellum, and between the two cerebral hemispheres, close to the centre of the brain. It contains the pineal gland, a small endocrine gland that produces the hormone melatonin, which controls circadian rhythms, or sleep-wake cycles.
Pineal Region Tumors: What Are They?
Less than 1% of all brain Tumors are pineal area Tumors, making them extremely uncommon. The pineal gland itself or nearby tissues including brain tissue, meninges, or germ cells may give rise to these Tumors.
Typical Pineal Region Tumor Types:
- The most prevalent malignant Tumor in this region is a germinoma.
- Benign and slowly developing pineocytomas
- Pineoblastomas (aggressive, high grade)
- Teratomas
- Gliomas
- Meningiomas
- Mixed germ cell Tumors and atypical Tumors
Why Do Pineal Tumors Occur?
The majority of pineal Tumors occur irregularly, which means their source is unknown.
Nevertheless, genetic changes that lead to abnormal or confused cells growing out of control can result in pineal Tumors. They may also result from abnormalities in the development of the embryo. Germ cells, for instance, usually move to develop into reproductive organs. However, some of these cells may subsequently grow into Tumors if they stay in the brain.
Even though they are uncommon, some pineal Tumors are linked to genetic disorders such as Li-Fraumeni Syndrome, which is brought on by TP53 gene abnormalities, or retinoblastoma, a rare and rapidly spreading hereditary eye cancer. Your risk of developing brain Tumors may be elevated by either of these hereditary diseases.
Pineal Region Tumor Symptoms
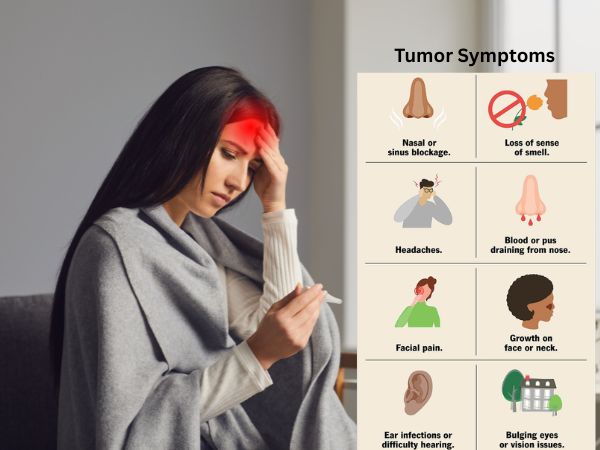
Because of the pineal gland’s deep location and close closeness to important brain areas, even small Tumors can produce serious symptoms like:
- Headache (caused by hydrocephalus or elevated intracranial pressure)
- Vomiting and feeling nauseous
- Parinaud’s syndrome, a defining feature of pineal Tumors, is the inability to move the eyes upward.
- Double or blurred vision
- Unbalanced or poorly coordinated
- Less common seizures
- Endocrine disorders (caused by melatonin or hormone pathway imbalance)
Diagnostics of Pineal Tumors
Neurological examinations, imaging studies, and laboratory work are frequently used in the diagnosis of pineal Tumors.
When diagnosing a pineal Tumor, the following instruments are frequently employed:
- Physical and neurological examination: Your doctor will first enquire about your general health, symptoms, and any potential risk factors. They will then conduct an examination to evaluate your neurological function, including reflexes, strength, coordination, sensation, and eye movements. This is because some problems with eye motions may indicate abnormalities in the pineal region.
- Ophthalmologic examination: An eye specialist may be called upon to assess your visual acuity and search for indications of elevated intracranial pressure, as pineal Tumors are known to cause symptoms connected to vision.
- The main imaging technique for detecting and diagnosing pineal Tumors is magnetic resonance imaging (MRI), which produces fine-grained images of the brain that can be used to determine the location, size, and features of a Tumor. To distinguish the Tumor from the surrounding tissues and assess its spread, an MRI with contrast may be utilised.
- Computed Tomography (CT): A CT scan uses X-rays to produce fine-grained cross-sectional brain images that aid in determining the size and location of a Tumor, even though an MRI is frequently the first option in neuroimaging. Additionally, calcifications, which are typical of pineal Tumors, and hydrocephalus can be detected using CT scans.
- A spinal tap, sometimes referred to as a lumbar puncture, is a procedure in which a needle is placed into the lower back to draw cerebrospinal fluid (CSF) in order to check for the presence of malignant cells. If your Tumor has spread throughout the central nervous system (CNS), this test can identify it.
- Blood tests: Certain pineal Tumors, especially germ cell Tumors, emit high levels of beta-human chorionic gonadotropin (hCG) or alpha-fetoprotein (AFP) in the blood or cerebrospinal fluid (CSF), which aids in the diagnosis of certain pineal Tumors.
- Biopsy: A biopsy is required if your imaging results point to a Tumor. A tiny sample is taken from the Tumor during a biopsy and sent to a pathology lab for examination. In order to identify the sort of cells present and other crucial features that inform treatment choices, pathologists there look at the tissue under a microscope. A biopsy is usually performed surgically or via stereotactic biopsy for brain Tumors.
Depending on the nature and degree of your pineal Tumor, more testing might be required.
Options for Treatment
The tumor’s nature, size, location, and grade, as well as the patient’s general condition, all influence the treatment plans.
- Observation
If small, benign Tumors like pineocytomas are not causing symptoms, they can be tracked with routine imaging.
- Resection via Surgery
- Recommended for huge, symptomatic, or accessible Tumors.
- Techniques include endoscopic, transcallosal, and infratentorial supracerebellar techniques.
- Hydrocephalus can also be relieved surgically (e.g., by conducting an endoscopic third ventriculostomy or installing a ventriculoperitoneal shunt).
- Treatment with Radiation
- Used frequently for malignant Tumors such as pineoblastomas or germinomas after surgery.
- Can be applied as the main course of treatment for some Tumors that are susceptible to radiation.
- The use of chemotherapy
- Very useful for germ cell Tumors.
- Frequently used in combination with radiation therapy for a better outcome.
Gamma Knife in Tumors of the Pineal Region
A non-invasive therapeutic method called Gamma Knife radiosurgery uses concentrated gamma radiation beams to target brain Tumors with sub-millimeter precision. It works particularly well for Tumors that are deep, difficult to access, or still present in the pineal region.
Gamma Knife Radiosurgery Advantages:
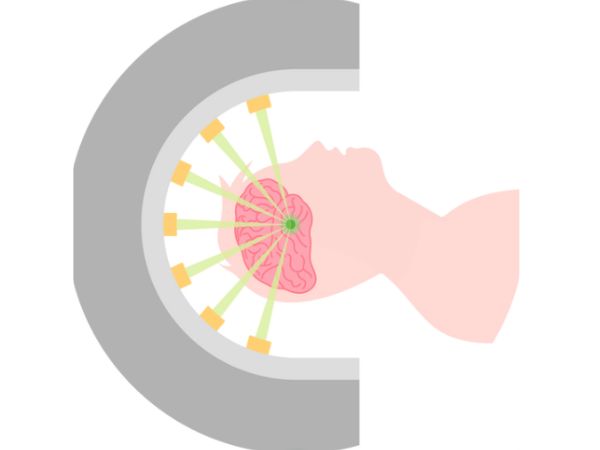
- Minimally invasive: doesn’t require general anaesthesia or incisions.
- Targeted precisely: Preserves the area around healthy brain tissue.
- Quick recovery: Frequently carried out as an outpatient operation.
- Perfect for little or persistent Tumors following surgical excision.
- Low incidences of complications.
Gamma Knife Indications for Pineal Tumors:
- Tumors that are inoperable or inaccessible during surgery.
- Unsuitable patients for open surgery.
- Recurring Tumors following the first radiation or surgery.
- Tumor tissue that remains after partial resection.
- Adjunct therapy for low-grade gliomas, meningiomas, and pineocytomas.
Restrictions:
- Not appropriate for big Tumors that cause hydrocephalus or a substantial bulk effect.
- Delayed Tumor shrinkage—it could take weeks or months to see results.
The outlook
Depending on the form and grade of the Tumor, the prognosis for pineal area Tumors varies greatly:
- With combination chemotherapy and radiation, germinomas have a very good prognosis (cure rates of over 90%).
- When removed surgically, pineocytomas have a favourable prognosis.
- Despite multimodal treatment, high-grade gliomas and pineoblastomas have a guarded prognosis and are more aggressive.
- Results are greatly enhanced by early diagnosis and individualised therapy, including radiosurgery.
In Conclusion
Despite being uncommon, pineal area Tumors necessitate a comprehensive approach from radiation specialists, neurosurgeons, neuro-oncologists, and radiologists. Patients now have access to precise, efficient, and minimally invasive choices thanks to advancements like Gamma Knife radiosurgery, which improves survival and quality of life.
Better results may result from early evaluation by a specialised neurosurgery team if you or a loved one has been diagnosed with a pineal area Tumor. To deliver individualised, evidence-based care, AIIMS Delhi is equipped with cutting-edge diagnostic and therapeutic instruments, such as Gamma Knife technology.
Sources:
- https://pmc.ncbi.nlm.nih.gov/articles/PMC8036741/
- https://www.cancer.gov/rare-brain-spine-tumor/tumors/pineal-region-tumors
- https://www.ncbi.nlm.nih.gov/books/NBK560567/
- https://www.barrowneuro.org/condition/pineal-tumors/
- https://www.webmd.com/brain/what-to-know-about-pineal-tumors
- https://emedicine.medscape.com/article/249945-overview?form=fpf
- https://www.cancerresearchuk.org/about-cancer/brain-Tumors/types/pineal-region-Tumors
- https://radiopaedia.org/articles/pineal-region-mass
- https://pmc.ncbi.nlm.nih.gov/articles/PMC4617952/
- https://pubmed.ncbi.nlm.nih.gov/18081477/
- https://www.jkns.or.kr/journal/view.php?number=1820
- https://www.jkns.or.kr/upload/pdf/0042006160.pdf
You May Also Know Related to Gamma Knife
FAQ’s
How does Gamma Knife work?
Gamma Knife uses 192–201 precisely focused beams of gamma rays that converge at a single target point in the brain. This high dose of radiation damages the DNA of abnormal cells, stopping their growth or causing them to shrink, while minimizing exposure to nearby healthy tissue.
Is Gamma Knife a surgery?
No, Gamma Knife is not a traditional surgery. It is a non-invasive outpatient procedure performed without any incision, stitches, or general anesthesia in most cases.
What conditions can be treated with Gamma Knife?
Gamma Knife is commonly used for:
Brain tumors (benign and malignant)
Metastatic brain lesions
Arteriovenous malformations (AVMs)
Trigeminal neuralgia
Acoustic neuromas (vestibular schwannomas)
Pituitary tumors
Certain functional disorders (like tremors)
Is Gamma Knife painful?
The procedure is generally painless. Patients may feel mild pressure while the head frame (if used) is applied or may experience slight discomfort from anesthesia injections, but the treatment itself is not painful.
How long does the procedure take?
Depending on the condition and treatment plan, Gamma Knife may take 30 minutes to 3 hours. Most patients go home the same day.
What are the possible side effects?
Common side effects are usually mild and temporary, including:
Headache
Nausea
Fatigue
Mild scalp swelling or tenderness at the frame site
Rarely, some patients may experience delayed radiation effects such as brain swelling or radiation necrosis.
When can the patient return to normal activities after Gamma Knife?
Most patients can return to their normal routine within 24–48 hours after the procedure.
You may feel mild fatigue for a few days.
Follow-up imaging is usually required after 1 year.
How effective is Gamma Knife?
Gamma Knife has a high success rate and has been used worldwide for decades. Its effectiveness depends on the condition treated, size and location of the lesion, and overall patient health. In many cases, it offers results comparable to open surgery with fewer risks.
Can Gamma Knife be repeated if needed?
Yes, in some cases Gamma Knife treatment can be repeated if the disease recurs or if new lesions develop.
Is Gamma Knife safe?
Yes. Gamma Knife is considered one of the safest and most precise forms of radiosurgery, with millions of patients treated globally and extensive clinical data supporting its use.
Who is eligible for Gamma Knife treatment?
Eligibility depends on factors such as:
Size and location of the lesion
Overall health and age
Whether open surgery is too risky
A neurosurgeon and radiation oncologist will decide if Gamma Knife is the best option for you.
What happens before the procedure?
A detailed MRI or CT scan is performed to map the brain.
A lightweight head frame or mask is used for accuracy.
Your doctors plan the radiation dose and target areas using specialized software.
Will I need anesthesia?
Local anesthesia is given if a head frame is used.
General anesthesia is usually not required, except for children or patients unable to remain still.
What is the cost of Gamma Knife in India?
Costs vary depending on hospital, city, and condition treated. On average, Gamma Knife in India ranges from ₹1.5 lakh to ₹4.5 lakh. It is usually more affordable compared to treatment in Western countries. At AIIMS Delhi, it is much more affordable around ₹75,000 which makes it affordable for the patients in need.
Where can I get Gamma Knife treatment in Delhi?
AIIMS Delhi is one of the leading centres for Gamma Knife in India.
AIIMS uses the latest Gamma Knife Perfexion system.
It has successfully treated thousands of patients for brain tumors, blood vessel problems, and even eye cancers.
The treatment is done by expert neurosurgeons such as Dr. Deepak Agrawal and team.
Clinic timings for Gamma Knife OPD at AIIMS Delhi: Monday & Friday, 8:00 AM – 9:00 AM.
Cost is around ₹75,000 and is subsidized compared to private hospitals.
What is the complete process of the Gamma Knife?
The whole procedure is usually done in one day:
- Consultation & Planning – Doctors review your scans and decide the treatment.
- Head Frame/Mask – A lightweight frame or mask is placed to keep your head still.
- Imaging – MRI/CT scans are done to locate the exact target.
- Treatment Planning – Specialists plan the dose and direction of radiation.
- Gamma Knife Treatment – You lie on the machine; painless radiation beams treat the target (30 mins–3 hrs).
- Recovery & Discharge – The frame is removed, and most patients go home the same day.
- Follow-up – MRI after a few months to check results.
What formalities do I have to complete prior to getting the date of GK?
Before you get a treatment date, you need to complete a few steps:
- OPD Registration – Visit the Neurosurgery OPD (Gamma Knife clinic at AIIMS, Mon & Fri 8–9 AM) and register.
- Consultation with Doctor – Meet the neurosurgeon who will check your reports, MRI/CT scans, and medical history.
- Investigations – Sometimes fresh MRI/CT or blood tests are needed for treatment planning.
- Medical Fitness – Basic checks like blood pressure, sugar, heart condition, etc.
Financial/Insurance Approval –
- If using Ayushman Bharat or government schemes, you need approval papers.
- If self-paying, you will be given the estimated cost (~₹75,000 at AIIMS).
- Consent & Admission Slip – Once doctors confirm you are fit and formalities are done, you sign the consent form.
- Treatment Date Allotment – A date is given for your Gamma Knife procedure.
What formalities do I have to complete after getting the date of GK?
Once you receive your Gamma Knife date, you’ll need to do a few simple things before the procedure:
- Admission Process – Report to AIIMS on the morning of your procedure and complete admission at the Neurosurgery ward/Daycare.
- Paperwork – Carry your OPD slip, MRI/CT films, blood test reports, admission slip, and ID proof. If you are covered under Ayushman Bharat/insurance, keep those approval papers ready.
- Consent Forms – You (or a family member) will sign consent for the procedure and anesthesia.
- Medical Check-up – Doctors will check your BP, sugar, heart rate, and do a quick physical exam.
- Fasting – Usually, you will be asked to not eat or drink for 6 hours before the procedure.
- Pre-Procedure Prep – An IV line may be put, and medicines (sedation/antibiotics if needed) are given.
- Treatment – You are then taken to the Gamma Knife room for frame/mask placement, imaging, and treatment.
After the procedure, you’ll be observed for a few hours and most patients are discharged the same day or next morning.
What investigations to be done?
Urea & creatinine
Should I come fasting?
No, You can have light breakfast.
In case of HT/DM should take my medicines?
Yes, you can take the medicine and then come for the treatment.