Topics
Table of Contents
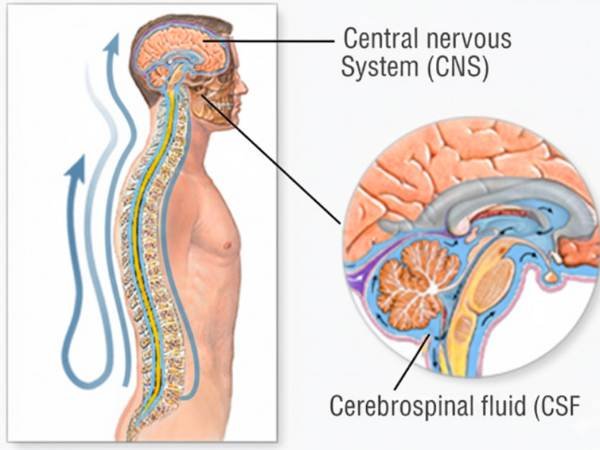
The way we comprehend and treat disorders of the brain and spinal cord is evolving due to advances in medical science. Stem cell treatment is one such promising field. Many patients and their families hear about stem cells, but they don’t know what they are, how they function, or if they are safe or beneficial.
In order to help patients make educated decisions, this page provides an easy-to-understand explanation of stem cells and their function in neurology.
Stem Cells: What Are They?
The body’s unique stem cells have the capacity to:
- Develop into several cell types
- Repair tissues that are injured
- Aid in the regeneration of organs and structures
Under the correct circumstances, stem cells can differentiate into nerve cells, supporting brain cells, or spinal cord cells, in contrast to normal cells like skin or muscle cells.
Why Do Stem Cells Matter in Neuroscience?
There is virtually little natural healing capacity in the brain and spinal cord. Nerve tissue frequently does not repair on its own after being harmed by an illness, injury, or stroke.
Hope is provided by stem cells since they may:
- Replacing injured nerve cells
- Encourage the restoration of brain and spinal cord function
- Decrease inflammation and aid in the recovery of neurological disorders
Stem Cell Types Used in Neuroscience
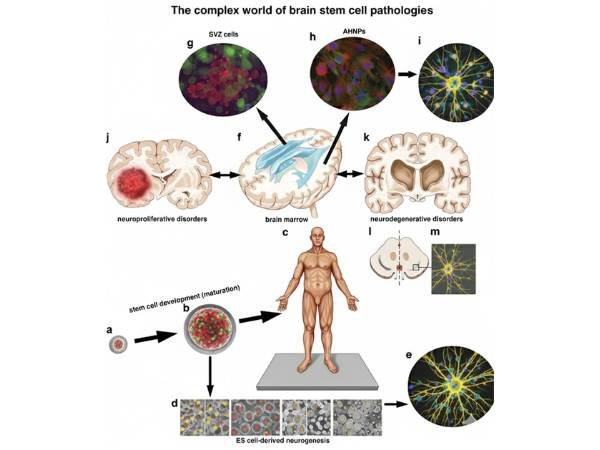
Stem cells from embryos
- Originating from early-stage embryos
- Can develop into any kind of cell.
- Primarily utilised in studies rather than standard healthcare procedures
- Widespread use is restricted by ethical considerations.
Somatic Adult Stem Cells
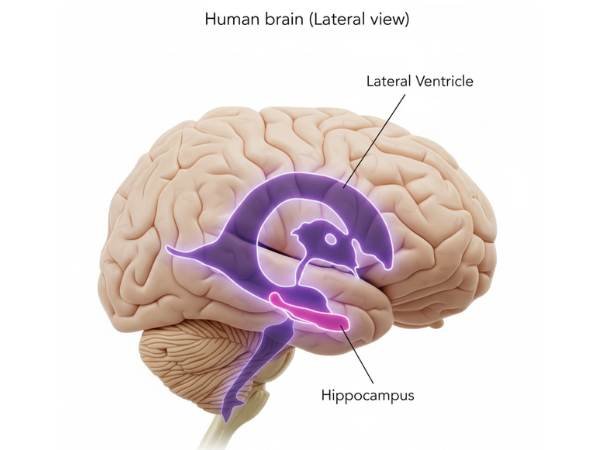
Located in:
- Bone marrow
- Blood
- Fat tissue
These are the stem cells that are most frequently researched for neurological disorders.
iPSCs, or induced pluripotent stem cells
- Reprogramming adult cells to act like embryonic stem cells
- A significant field of current study
- Not yet extensively utilised in standard patient care
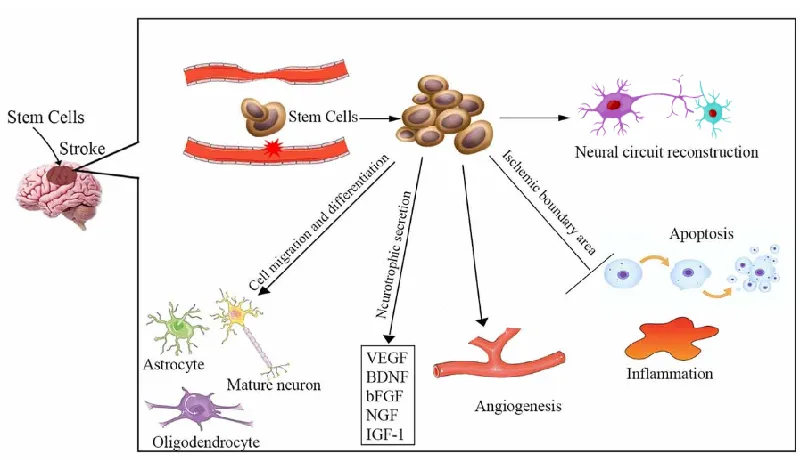
How Do Stem Cells Help with Disorders of the Brain and Spine?
- Stem cells could be useful by:
- Replacing damaged nerve cells
- Support current neurones
- Decreasing the amount of scar tissue
- Growth factors that promote healing are released
It is crucial to realise that while stem cells cannot “cure” neurological disorders right away, they may aid in recovery and, in certain situations, slow down the disease’s progression.
Research on Neurological Disorders for Stem Cell Treatment
Research on stem cells is being conducted in circumstances like:

- Stroke
- Traumatic Brain Injury (TBI)
- Spinal Cord Injury
- Parkinson’s illness
- Alzheimer’s
- Multiple Sclerosis
- Brain Palsy
- ALS, or motor neurone disease
Note: The majority of these treatments are not yet routine care and are still in clinical studies.
Are Treatments Using Stem Cells Clinically Proven?
Currently:
- In neurology, stem cell therapy is mostly experimental.
- Benefits are only demonstrated in small, carefully monitored clinical trials.
- Brain or spinal problems cannot be cured with stem cell therapy.
Clinics that promise “miracle cures” or “100% recovery” should be avoided by patients.
Is the Use of Stem Cells Safe?
Risks are reduced when carried out in accordance with regulated medical guidelines or approved clinical studies.
Potential dangers consist of:
- Infection
- Immune responses
- Unusual growth of cells
- No reduction in symptoms
That’s why ethical clearance, medical supervision, and appropriate patient selection is very important.
For whom is stem cell therapy an option?
Potential uses for stem cell therapy include:
- Patients who are not improving with traditional therapies
- Individuals eligible for clinical trials
- Carefully chosen instances following professional neurological assessment
Before considering any such procedure, consultation with a neurosurgeon is essential.
Neurosurgeons Contribution in Stem Cell Research
Neurosurgeons play a crucial role in:
- Finding appropriate patients
- Safe delivery of stem cells to the brain or spinal cord
- Tracking results and issues
- Participating in scientific and ethical research
Stem Cells Prospects in Neuroscience
Research is still being conducted globally to:
- Boost efficacy and safety
- Recognise the long-term advantages
- Create individualised treatments
- Combine stem cells with advanced surgery and recovery.
Stem cells offer hope for the future, but their application must be guided by research rather than hype.
Crucial Information for Families and Patients
In neurology, stem cell therapy is a promising but developing subject. Even while it gives hope, it must be handled with scientific cautiousness, moral responsibility, and professional medical advice.
Before considering any kind of stem cell treatment, always speak with a professional neurosurgeon.
FAQ’s
Can brain injury or paralysis be treated with stem cells?
As of right now, a cure is not assured. Although outcomes vary greatly, some people may see a partial improvement.
Does India allow stem cell therapy?
The only approved stem cell treatments are those undergoing clinical studies. Avoiding commercial uncontrolled therapy is advised.
How is stem cell treatment administered?
Depending on the illness, stem cells could be:
- Injected into the spinal fluid
- Delivered close to the source of harm
- Administered intravenously (in certain studies)
Does stem cell treatment cause pain?
The majority of procedures are painless because they are often performed under general or local anaesthesia.
Do adverse effects occur?
Infection, fever, inflammation, or no improvement are potential hazards. When done correctly, serious problems are uncommon.
How much time does it take to see results?
If progress is made, rehabilitation and improvement may take weeks or months.
Is stem cell treatment costly?
Prices vary greatly, particularly for experimental treatments. Financial concerns should always be discussed in advance with patients.
Should I believe commercials that promise outcomes?
No, results are never guaranteed by ethical medical practice, particularly when it comes to experimental treatments.
Is it possible to combine stem cell therapy with rehabilitation or surgery?
Indeed. If stem cell therapy is employed, it is frequently paired with neurosurgery, physical therapy, occupational therapy, and rehabilitation. In order to maximise any possible benefit from stem cell treatment, rehabilitation is essential.
Do stem cells come from a donor or from my own body?
Depending on the type of therapy and research technique, stem cells can be taken from a donor source or from the patient’s own body (autologous stem cells), usually from bone marrow or fat. Rejection is typically less likely when using one’s own stem cells.
Sources:
- https://pmc.ncbi.nlm.nih.gov/articles/PMC11416137/
- https://www.brainandspineni.com/blog/stem-cell-treatment-and-neurological-disorders/
- https://www.sciencedirect.com/science/chapter/edited-volume/abs/pii/B9780128217764000123
- https://www.stemcell.com/technical-resources/area-of-interest/neuroscience-research/neural-stem-cells/overview.html
- https://www.frontiersin.org/journals/molecular-medicine/articles/10.3389/fmmed.2025.1569717/full
- https://www.dvcstem.com/post/stem-cell-therapy-for-neurological-disorders
- https://pubmed.ncbi.nlm.nih.gov/39341661/
- https://pubmed.ncbi.nlm.nih.gov/10679764/
- https://pubmed.ncbi.nlm.nih.gov/15640745/
- https://pubmed.ncbi.nlm.nih.gov/35367733/