Topics
Table of Contents
The vertebral artery: what is it?

Two vertebral arteries travel along the back of your neck, close to the vertebrae, which make up your spine. They provide your brain and spine with blood that is rich in oxygen.
Three layers make up the vertebral artery:
- The innermost layer nearest blood flow is called the intima.
- The media is the intermediary layer that maintains proper blood flow.
- The outermost layer that provides blood vessels their structure is called the adventitia.
What health effects might vertebral artery dissection have?
Blood becomes caught between the media and intima during a dissection. Unmoving blood can clot, causing a bulge that stops the flow of blood. Additionally, it may cause the artery to dilate.
In the worst situations, stroke is brought on by vertebral artery dissection:
- When a clot is big enough to stop blood flow to the brain, an ischaemic stroke happens. Additionally, clots may separate, move through your bloodstream, and become lodged in an artery later on.
- When all three layers of arterial tissue are affected by a dissection, hemorrhagic stroke happens. As a result, blood leaks from the artery rather than into your brain. Your brain may bleed into the surrounding tissue (subarachnoid haemorrhage) or into itself if the dissection penetrates inside of it.
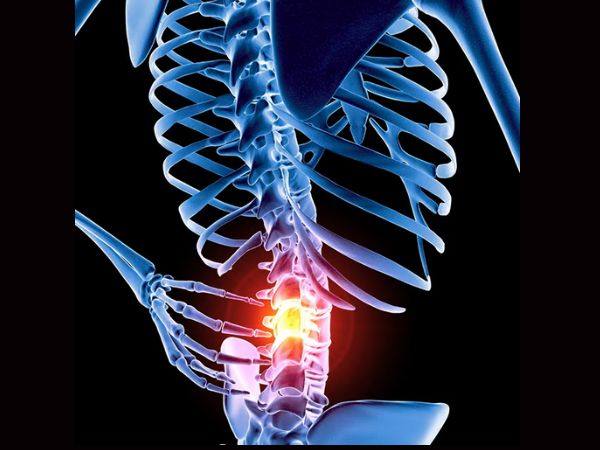
A rare but potentially fatal disorder, vertebral artery injury (VAI) has major consequences for trauma, cervical spine surgery, and skull base treatments. Because of its complex anatomical path and function in supplying the brain’s posterior circulation, damage to the vertebral artery can cause brainstem infarcts, strokes in the posterior circulation, or even death.
The use of high-resolution imaging methods like CT angiography (CTA) and MR angiography (MRA) has raised the detection rate of these injuries, which were previously underdiagnosed because of vague clinical signs. In order to reduce the chance of long-term neurological consequences, prompt diagnosis and prompt treatment are crucial.
There are two types of vertebral artery injuries: Traumatic and Spontaneous. Although penetrating trauma may sometimes be the cause, blunt injuries to the head and neck are the most common cause of traumatic injuries. A vessel dissection results from spontaneous injuries, which are brought on by the intrinsic weakness of the vessel wall, frequently as a result of an underlying vascular or connective tissue condition. The causes, pathophysiology, and diagnostics of vertebral artery injury are covered in this activity, which also emphasises the need of the interprofessional team in treating these patients.
Minor triggering factors are sometimes linked to spontaneous dissections. A defect of the artery wall or a complete transection with cerebral or extracranial haemorrhage are examples of different injury grades. Although they may not have any symptoms, patients frequently arrive with a headache and neck pain. Particularly in younger individuals, vertebral artery damage is a significant risk factor for stroke and transient ischaemic attack. The patient will exhibit stroke symptoms that are consistent with impairments in the posterior circulation because the posterior fossa is supplied with blood by the vertebral arteries. Having trouble speaking, swallowing, or staying balanced are some symptoms. There may also be alterations in vision or a loss of coordination. Patients at high risk for cerebrovascular injury are identified using the modified Denver screening criteria. The preferred first diagnostic imaging test is a CT angiography. Treatment options include fibrinolysis, anticoagulation, antiplatelet therapy, endovascular therapy, and open surgical repair, depending on the site, severity, and symptoms of the injury.
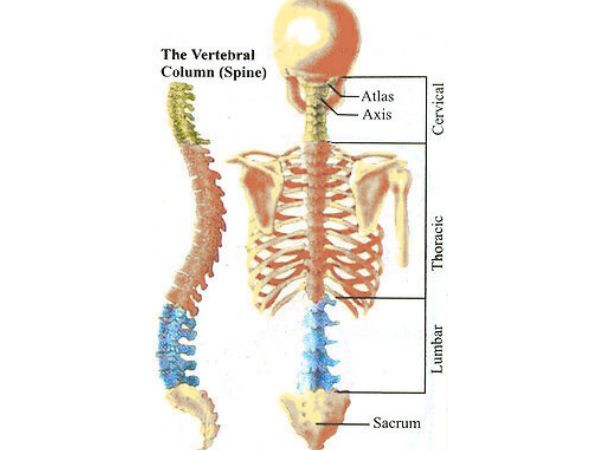
The Vertebral Artery Anatomy in DETAIL
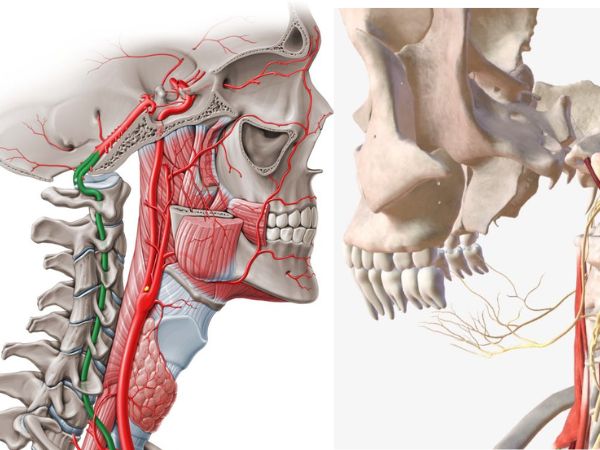
A significant branch of the subclavian artery, the vertebral artery (VA) supplies blood to the brainstem, cerebellum, upper spinal cord, and posterior cerebral hemispheres as part of the vertebrobasilar circulation.
There are four sections to its anatomical course:
Pre-Foraminal Segment, or V1 Segment:
- The subclavian artery is the source.
- Reaches the transverse foramen of C6 (but in certain people it may enter at C5 or C7).
- Located close to the scalenus anterior and longus colli muscles.
- At risk when the lower cervical spine is being surgically approached.
Formal Segment, or V2 Segment:
- Moves from C6 to C2 in a vertical direction through the transverse foramina.
- Although well-protected inside the bone canals, the cervical vertebrae are prone to fractures and dislocations.
Atlantoaxial/Extraspinal Segment, or V3 Segment:
- Appears as the artery leaves the C2 transverse foramen.
- Protects the atlas’ lateral bulk laterally and posteriorly (C1).
- Enters the foramen magnum by passing via the posterior arch of C1 and penetrating the dura mater and atlanto-occipital membrane.
- Extremely mobile and susceptible to changes in the Craniovertebral Junction (CVJ).
The intradural segment, or V4 segment:
- Generates the basilar artery by extending from the dural puncture at the foramen magnum to the point where it joins the contralateral VA.
- Supplies the posterior cerebrum, cerebellum, and medulla.
The pattern of dominance
- In over 50% of people, one VA may be dominant.
- One vertebral artery may be hypoplastic or even aplastic in roughly 10% to 15% of cases.
Causes and Mechanisms of Damage
Causes of Trauma:
Trauma Blunt:
- Sports injuries, car crashes, and height falls are examples of high-energy systems.
- May coexist with facet dislocations, subluxations, and cervical spine fractures, particularly those affecting the transverse foramen.
Trauma that penetrates:
- Direct injuries to the neck caused by sharp objects or weapons.
- Frequently results in arteriovenous fistula, pseudoaneurysm, or transection.
Rotational or hyperextensional injuries:
- May result in dissection and intimal disruption, especially in the mobile V3 segment.
Chiropractic Adjustments:
- A rare but well-documented cause of dissection is sudden rotational forces or hyperextension.
Latrogenic Factors:
Surgery for the Cervical Spine:
- VAI can result with both anterior and posterior cervical spine techniques, particularly corpectomy or instrumentation close to the transverse foramen.
Surgery for CVJ:
- Decompression techniques for basilar invagination or Chiari malformation.
Surgery on the Skull Base and Posterior Fossa:
- The intradural section (V4) may be at risk from retrosigmoid or far-lateral approaches.
Endovascular Techniques:
- Dissection or embolism may result with catheter manipulation.
The reason for all:
- Luminal narrowing or occlusion is a sign of intimal tear and dissection.
- Formation of Pseudoaneurysm: Focal arterial wall dilatation.
- A posterior circulation stroke may result from thromboembolism.
- Abnormal connection with venous structures is known as an arteriovenous fistula.
- Complete Transection: Haemorrhage that could be lethal.
Clinical Demonstration
No symptoms/ Asymptomatic:
- Frequently silent, particularly when the collateral supply or non-dominant artery is intact.
Indicative/ Symptomatic:
- Stroke in the posterior circulation
- Vertigo, ataxia, and occipital headache
- Horner’s syndrome, dysphagia, and diplopia
- In extreme situations, syncope or death
Methods of Diagnosis
- CT Angiography (CTA): High-resolution, first-line, and quick.
- For intimal damage, MR Angiography (MRA) is beneficial.
- The gold standard, digital subtraction angiography (DSA), enables intervention.
- Limited but helpful for follow-up is ultrasound.
- Denver and Memphis screening standards in trauma situations.
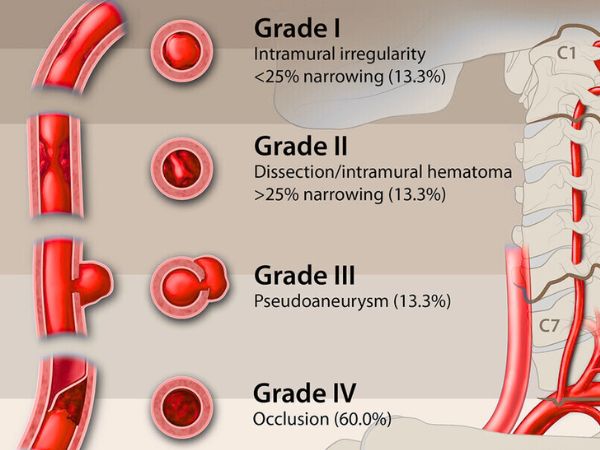
Vertebral Artery Injury classification
The Biffl Scale
| Grade | An explanation |
|---|---|
| I | Less than 25% constriction in luminal irregularity |
| II | Dissection >25% reduction in width |
| III | Pseudoaneurysm |
| IV | Occlusion |
| V | Extravasation combined with transection |
Strategies for Management
- Health/Medical:
- Antiplatelets: For Grades I–II minor wounds.
- Anticoagulation: For embolic episodes or dissections.
- Serial imaging is used for monitoring.
- Endovascular
- For dissections, AVFs, or pseudoaneurysms, use stents, coiling, or occlusion.
- Surgical:
- Ligation, repair, or bypass: Saved for bleeding that is unmanageable or inaccessible.
Results and Prognosis
- Early diagnosis and modest damage are indicators of a good prognosis.
- Poor prognosis: delayed treatment, bilateral injuries.
- Mortality: according on severity, 10–25%.
- Sequelae: Deficits associated with stroke.
In conclusion:
In neurosurgery and trauma care, vertebral artery damage or injury is still a low-incidence, high-risk condition. To avoid adverse effects, a proactive strategy combining anatomical knowledge, risk assessment, attentive imaging, and customised intervention techniques is necessary. In order to manage this difficult situation, interdisciplinary cooperation between neurosurgeons, neuroradiologists, and trauma specialists guarantees the best results.
Know More: Childhood Trauma: Types, Causes, Signs, and Treatments
Sources:
- https://pubmed.ncbi.nlm.nih.gov/33470592/
- https://pubmed.ncbi.nlm.nih.gov/18504163/
- https://pubmed.ncbi.nlm.nih.gov/21674212/
- https://my.clevelandclinic.org/health/diseases/23961-vertebral-artery-dissection
- https://www.ncbi.nlm.nih.gov/books/NBK470363/#:~:text=In%20most%20cases%2C%20vertebral%20artery,circulation%20resulting%20in%20a%20stroke.
- https://www.sciencedirect.com/science/article/pii/S2352644023000286
- https://www.polradiol.com/Traumatic-vertebral-artery-injury-a-review-of-the-screening-criteria-imaging-spectrum,109122,0,2.html
- https://www.orthobullets.com/spine/12785/vertebral-artery-injury
You May Also Know Related to Gamma Knife
FAQ’s
How does Gamma Knife work?
Gamma Knife uses 192–201 precisely focused beams of gamma rays that converge at a single target point in the brain. This high dose of radiation damages the DNA of abnormal cells, stopping their growth or causing them to shrink, while minimizing exposure to nearby healthy tissue.
Is Gamma Knife a surgery?
No, Gamma Knife is not a traditional surgery. It is a non-invasive outpatient procedure performed without any incision, stitches, or general anesthesia in most cases.
What conditions can be treated with Gamma Knife?
Gamma Knife is commonly used for:
Brain tumors (benign and malignant)
Metastatic brain lesions
Arteriovenous malformations (AVMs)
Trigeminal neuralgia
Acoustic neuromas (vestibular schwannomas)
Pituitary tumors
Certain functional disorders (like tremors)
Is Gamma Knife painful?
The procedure is generally painless. Patients may feel mild pressure while the head frame (if used) is applied or may experience slight discomfort from anesthesia injections, but the treatment itself is not painful.
How long does the procedure take?
Depending on the condition and treatment plan, Gamma Knife may take 30 minutes to 3 hours. Most patients go home the same day.
What are the possible side effects?
Common side effects are usually mild and temporary, including:
Headache
Nausea
Fatigue
Mild scalp swelling or tenderness at the frame site
Rarely, some patients may experience delayed radiation effects such as brain swelling or radiation necrosis.
When can the patient return to normal activities after Gamma Knife?
Most patients can return to their normal routine within 24–48 hours after the procedure.
You may feel mild fatigue for a few days.
Follow-up imaging is usually required after 1 year.
How effective is Gamma Knife?
Gamma Knife has a high success rate and has been used worldwide for decades. Its effectiveness depends on the condition treated, size and location of the lesion, and overall patient health. In many cases, it offers results comparable to open surgery with fewer risks.
Can Gamma Knife be repeated if needed?
Yes, in some cases Gamma Knife treatment can be repeated if the disease recurs or if new lesions develop.
Is Gamma Knife safe?
Yes. Gamma Knife is considered one of the safest and most precise forms of radiosurgery, with millions of patients treated globally and extensive clinical data supporting its use.
Who is eligible for Gamma Knife treatment?
Eligibility depends on factors such as:
Size and location of the lesion
Overall health and age
Whether open surgery is too risky
A neurosurgeon and radiation oncologist will decide if Gamma Knife is the best option for you.
What happens before the procedure?
A detailed MRI or CT scan is performed to map the brain.
A lightweight head frame or mask is used for accuracy.
Your doctors plan the radiation dose and target areas using specialized software.
Will I need anesthesia?
Local anesthesia is given if a head frame is used.
General anesthesia is usually not required, except for children or patients unable to remain still.
What is the cost of Gamma Knife in India?
Costs vary depending on hospital, city, and condition treated. On average, Gamma Knife in India ranges from ₹1.5 lakh to ₹4.5 lakh. It is usually more affordable compared to treatment in Western countries. At AIIMS Delhi, it is much more affordable around ₹75,000 which makes it affordable for the patients in need.
Where can I get Gamma Knife treatment in Delhi?
AIIMS Delhi is one of the leading centres for Gamma Knife in India.
AIIMS uses the latest Gamma Knife Perfexion system.
It has successfully treated thousands of patients for brain tumors, blood vessel problems, and even eye cancers.
The treatment is done by expert neurosurgeons such as Dr. Deepak Agrawal and team.
Clinic timings for Gamma Knife OPD at AIIMS Delhi: Monday & Friday, 8:00 AM – 9:00 AM.
Cost is around ₹75,000 and is subsidized compared to private hospitals.
What is the complete process of the Gamma Knife?
The whole procedure is usually done in one day:
- Consultation & Planning – Doctors review your scans and decide the treatment.
- Head Frame/Mask – A lightweight frame or mask is placed to keep your head still.
- Imaging – MRI/CT scans are done to locate the exact target.
- Treatment Planning – Specialists plan the dose and direction of radiation.
- Gamma Knife Treatment – You lie on the machine; painless radiation beams treat the target (30 mins–3 hrs).
- Recovery & Discharge – The frame is removed, and most patients go home the same day.
- Follow-up – MRI after a few months to check results.
What formalities do I have to complete prior to getting the date of GK?
Before you get a treatment date, you need to complete a few steps:
- OPD Registration – Visit the Neurosurgery OPD (Gamma Knife clinic at AIIMS, Mon & Fri 8–9 AM) and register.
- Consultation with Doctor – Meet the neurosurgeon who will check your reports, MRI/CT scans, and medical history.
- Investigations – Sometimes fresh MRI/CT or blood tests are needed for treatment planning.
- Medical Fitness – Basic checks like blood pressure, sugar, heart condition, etc.
Financial/Insurance Approval –
- If using Ayushman Bharat or government schemes, you need approval papers.
- If self-paying, you will be given the estimated cost (~₹75,000 at AIIMS).
- Consent & Admission Slip – Once doctors confirm you are fit and formalities are done, you sign the consent form.
- Treatment Date Allotment – A date is given for your Gamma Knife procedure.
What formalities do I have to complete after getting the date of GK?
Once you receive your Gamma Knife date, you’ll need to do a few simple things before the procedure:
- Admission Process – Report to AIIMS on the morning of your procedure and complete admission at the Neurosurgery ward/Daycare.
- Paperwork – Carry your OPD slip, MRI/CT films, blood test reports, admission slip, and ID proof. If you are covered under Ayushman Bharat/insurance, keep those approval papers ready.
- Consent Forms – You (or a family member) will sign consent for the procedure and anesthesia.
- Medical Check-up – Doctors will check your BP, sugar, heart rate, and do a quick physical exam.
- Fasting – Usually, you will be asked to not eat or drink for 6 hours before the procedure.
- Pre-Procedure Prep – An IV line may be put, and medicines (sedation/antibiotics if needed) are given.
- Treatment – You are then taken to the Gamma Knife room for frame/mask placement, imaging, and treatment.
After the procedure, you’ll be observed for a few hours and most patients are discharged the same day or next morning.
What investigations to be done?
Urea & creatinine
Should I come fasting?
No, You can have light breakfast.
In case of HT/DM should take my medicines?
Yes, you can take the medicine and then come for the treatment.