Topics
Table of Contents
One of the most severe but uncommon brain ailments in humans is Creutzfeldt-Jakob Disease (CJD). Even though many people are unaware of it, knowing its early symptoms and diagnosis can enable patients, carers, and families to seek prompt assistance and care. This guide describes CJD, including its early symptoms, progression, difficulties in diagnosis, available treatments, and the importance of family counselling.
CJD: What is it?
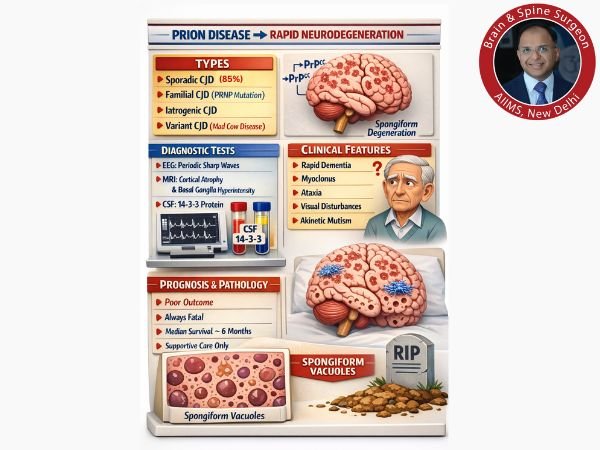
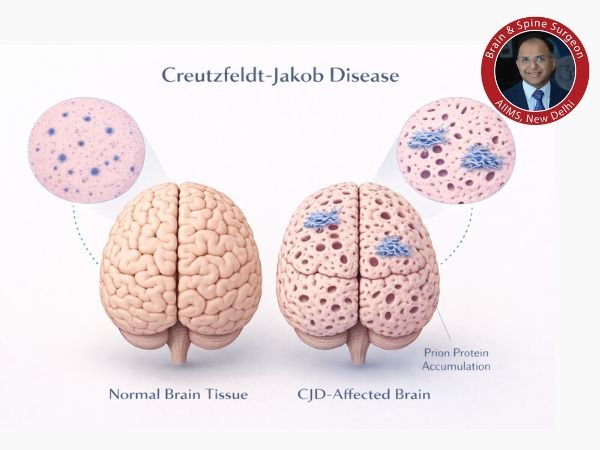
A rare, progressive, and deadly neurological disorder that affects the brain is called Creutzfeldt-Jakob Disease (CJD). It is a member of a class of illnesses known as prion diseases, which are brought on by aberrant proteins called prions that build up in the brain and harm nerve cells. Under a microscope, this results in fast neurodegeneration and the distinctive “spongy” look of brain tissue. CJD primarily affects older folks and affects about 1-2 people per million worldwide each year.
Related Post: Prion Disease: Symptoms, Causes, Types, & Treatment
CJD comes in a variety of forms:
The most prevalent type of CJD, sporadic, has no recognised cause.
Genetic mutations that are inherited cause familial CJD.
Latrogenic CJD: Extremely uncommon; formerly spread by contaminated medical equipment or procedures.
Variant CJD (vCJD): Rarely associated with prion infection from infected beef.
Early Signs of Neurology
The early stages of CJD frequently start slowly and can be mistaken for other illnesses, including mental disorders or Alzheimer’s disease. But compared to other dementias, it usually progresses far more quickly.
Typical initial symptoms consist of:
Cognitive impairment, or memory loss and deteriorating reasoning skills
Changes in behaviour and personality (emotional fluctuations, depression, anxiety)
Disorientation, confusion, or difficulty focusing
Issues with coordination and balance (ataxia)
Speech issues and difficulty swallowing
Blurred eyesight and visual disturbances
Changes in sleep patterns or insomnia
Later in the course, myoclonus, or involuntary muscular jerks, frequently happens.
Early detection is difficult since these symptoms can arise suddenly or gradually and are frequently mistaken for signs of stress or ageing.
Progression of the Disease

CJD usually advances quickly once symptoms start. CJD can worsen in a matter of weeks or months, in contrast to more prevalent dementias that take years to manifest.
As the illness progresses:
Severe dementia results from a worsening of cognitive decline.
Weakening muscle control results in involuntary motions and an unsteady walk.
Vision may continue to deteriorate, occasionally leading to blindness.
Patients may go into a coma, become bedridden, and lose their ability to swallow or speak.
The majority of people with classic CJD pass away within a year of the onset of symptoms, frequently as a result of problems like heart or respiratory failure, infections (like pneumonia), or both.
Diagnostic Difficulties
Since many of CJD’s symptoms resemble those of other neurological conditions, early diagnosis is difficult. While a person is still living, no single test can accurately identify CJD, and there isn’t a straightforward blood test to do so.
Among the diagnostic instruments are:
Neurological examination: Evaluating motor function, reflexes, and coordination.
Magnetic resonance imaging, or MRI, frequently reveals distinctive alterations in the brain.
In certain situations, an electroencephalogram (EEG) may show distinctively aberrant brainwave patterns.
Tests for cerebrospinal fluid (CSF) include protein measurements and specialised assays like RT-QuIC, which is very specific for prion disorders.
The only conclusive evidence is a brain biopsy, which is rarely done because of the risk.
As part of the diagnostic process, clinicians must rule out other disorders because the symptoms of CJD might mimic those of other curable conditions.
Treatment Options
As of right now, there is no cure for CJD nor a medication that can halt or reverse the disease’s course.
Symptom improvement and supportive care are the main goals of medical care:
Pain, anxiety, and muscle spasms may all be eased by medication.
Nutritional assistance and treatment for swallowing issues.
Palliative care or hospice to enhance quality of life in the latter stages.
Experimental treatments are being investigated as part of continuing research, but none have yet demonstrated a definite advantage in changing the course of the disease.
Counselling for Families
For both patients and their families, receiving a CJD diagnosis is a life-altering event. Since the illness is deadly and advances quickly, it becomes imperative to have open lines of communication and provide emotional support. Among the crucial elements of family counselling are:
Having a basic understanding of the diagnosis and prognosis
Making decisions about end-of-life care and hospice care
Taking care of carer exhaustion, grief, and psychological stress
If a familial type is suspected, talking about genetic concerns
Families can manage the practical and emotional difficulties of CJD with the assistance of counsellors and support groups.
Conclusion
Despite being uncommon, CJD has a significant impact. Families may seek professional care, make educated decisions, and find support during an incredibly difficult journey when they are aware of the early indications of CJD disease and comprehend the diagnostic procedures.
FAQ’s
1. How widespread is CJD?
CJD is incredibly uncommon, affecting just 1 to 2 individuals per million annually.
2. Is CJD communicable?
Common contact, such as touching, coughing, or kissing, does not transmit CJD. Although extremely rare, transmission has happened through tainted medical equipment or tissue.
3. Is it possible to avoid CJD?
There is no established preventive method due to its unknown causes, particularly in isolated occurrences. Iatrogenic danger is decreased by strict sterilisation and safe medical procedures.
4. What distinguishes Alzheimer’s illness from CJD?
Both cause dementia, but CJD has distinct neurological symptoms (such as myoclonus) and advances considerably more quickly—usually over months rather than years.
5. Is it possible to heal from CJD?
No recovery has been reported as of yet. Comfort and supportive care are the main goals of treatment.