Topics
Table of Contents
Endoscopic Endonasal Transsphenoidal Approach for Pituitary Adenoma
What is a Pituitary Tumor?
Unusual growths that form in the pituitary gland are known as pituitary tumours. The size of this gland looks similar to that of a pea. It is situated at the base of the brain, behind the nose. The pituitary gland produces too many hormones that regulate vital bodily processes as a result of certain of these tumours. Others may result in insufficient production of those hormones by the pituitary gland.
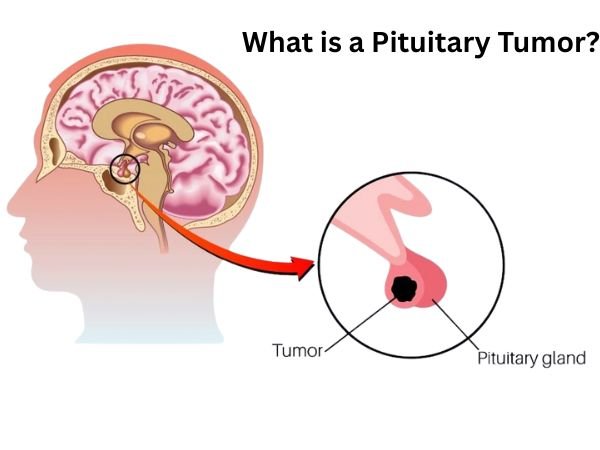
The majority of pituitary tumours are harmless. Thus, they are not cancer. Pituitary adenomas are another term for these benign tumours. The majority of adenomas grow slowly and remain in the pituitary gland or the tissue around it. Usually, they don’t spread to other bodily parts.
Treatment options for pituitary tumours are numerous. Surgery may be used to remove the tumour. Alternatively, radiation therapy or medication may be used to restrict its growth. Medicine is sometimes used to control hormone levels. A combination of these therapies may be recommended by the doctor. Sometimes the best course of action is observation, sometimes known as a “wait-and-see” strategy.
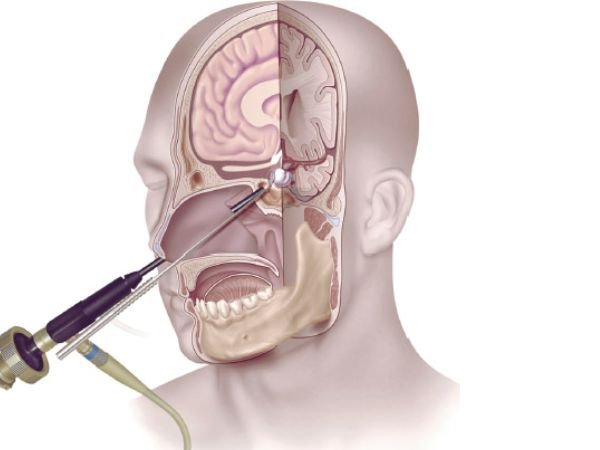
Through the nose and sphenoid sinus, the pituitary gland and surrounding tissues can be accessed using the endonasal transsphenoidal method, a minimally invasive surgical technique. This method is frequently used to treat disorders like acromegaly or Cushing’s disease, remove pituitary tumours, and correct other anomalies in the base of the skull.
Despite being benign, pituitary adenomas can have a significant impact on a patient’s health, resulting in everything from hormone abnormalities to vision impairment via optic chiasm compression. Pituitary surgery has been changed by the endoscopic endonasal transsphenoidal approach (EETA), which provides a less invasive method of tumour removal with fewer side effects and a quicker recovery.
Endoscopic endonasal surgery: What is it?
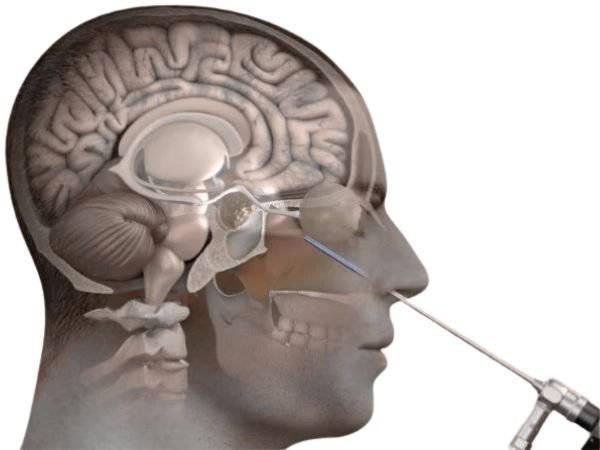
A cutting-edge technique called endoscopic endonasal surgery removes the need for open surgery by entering the nasal passages and accessing the pituitary gland and surrounding structures. This method enables surgeons to precisely view and access the surgical area by using a high-definition endoscope, a tiny, flexible tube equipped with a light and camera.
The endonasal technique removes brain tumours, numerous midline skull base tumours, and pituitary adenomas by using the nostrils as natural surgical passageways.
For practically all pituitary adenomas, Rathke’s cleft cysts, the majority of craniopharyngiomas, clival chordomas, and numerous midline menigiomas, the endonasal route is the recommended surgical technique. In skilled hands, the endonasal approach has become a safe and successful treatment that uses high-definition endoscopy (a surgical telescope), surgical navigation (sometimes known as “GPS for the brain”), and Doppler ultrasound for carotid artery localisation.
The main benefits of the endonasal approach:
- Avoiding brain retraction
- Requiring little to no treatment of the optic nerves
- Avoiding facial incisions
- Rarely requiring nasal packing
Endoscopic Endonasal Surgery: Advantages
When treating pituitary disorders, endoscopic endonasal surgery has a number of advantages over standard techniques.
These consist of:
- Minimally invasive: By performing the entire procedure through the nose, no exterior cuts are made, and the surrounding tissues are not as severely damaged.
- Faster recovery: In comparison to standard surgery, patients frequently report shorter hospital stays (48–72 hours post-surgery), less pain, and a quicker recovery in general.
- Better visualisation: The endoscope makes it easier to see the surgical site, which enables more accurate tumour removal and lowers the risk to adjacent vital tissues.
- Decreased risk of problems: Endoscopic endonasal surgery considerably reduces the risk of complications including infection and CSF leakage.
Knowing How to Use the Endoscopic Endonasal Method

In the past, microscopic transsphenoidal surgery or open craniotomy were used to access pituitary adenomas. However, direct visibility and improved mobility have been made possible by the development of endoscopic procedures, which has improved surgical results.
Using a high-definition endoscope, EETA involves getting into the pituitary gland through the sphenoid sinus and nostrils. By doing away with the necessity for external incisions, this method reduces post-operative morbidity and stress to the surrounding tissues.
The Preoperative Assessment of Endoscopic Endonasal Surgery
- Patients will have a thorough preoperative evaluation prior to endoscopic endonasal surgery, which may involve hormonal testing, imaging studies, and consultations with our experienced neurosurgeons and endocrinologists. This comprehensive evaluation guarantees personalised treatment programs targeted to the unique requirements of every patient.
Method of Surgery
- The patient is put under general anaesthesia for the procedure. With the help of an otolaryngologist, the neurosurgeon inserts the endoscope through the nostrils to reach the pituitary gland and its surroundings. While maintaining normal pituitary gland function, advanced tools and procedures are used to remove or treat the pituitary tumour or other underlying problems.
Recovery and Postoperative Care
- Before being moved to a hospital room after endoscopic endonasal surgery, patients are closely watched in the recovery area. Experienced medical staff offers complete postoperative care, including pain management, hormone level monitoring, and handling any possible complications. The majority of patients recover more easily and can resume their regular activities in 2-3 weeks.
- Patients are kept under observation for diabetes insipidus and hormone abnormalities, which may necessitate short-term hormone replacement treatment. Mild headaches and nasal congestion are frequent but go away in a few weeks.
The Surgical Procedure in Steps
- Patient Preparation: In order to schedule surgery, patients get CT and MRI scans. Vasoconstrictors are used to clear congestion in the nose in order to reduce bleeding.
- Nasal Entry: To view the sphenoid sinus, a rigid endoscope, typically 4 mm in diameter, is placed via one nostril.
- Sphenoidotomy: The sella turcica is revealed by delicately opening the sphenoid sinus’s anterior wall.
- Tumour Removal and Dural Opening: Using microsurgical tools, the adenoma is carefully removed once the dura is cut.
- Reconstruction: To stop cerebrospinal fluid (CSF) leakage, the sellar floor is reconstructed using synthetic materials or autologous tissue grafts.
Pituitary adenomas that can be accessed with the endoscopic endonasal approach include:
Pituitary adenomas including:
- Acromegaly
- Crushing’s Disease
- Prolactinomas
- TSH-Secreting Adenomas
- Non-Functional Adenomas
- Pituitary Apoplexy
- Recurrent Adenomas
Non-Pituitary Tumors
- Craniopharyngioma
- Rathke’s Cleft Cyst
- Sellar Arachnoid Cyst
- Meningioma (tuberculum sellae, parasellar, cavernous sinus regions)
- Clival Chordoma
- Sinonasal Carcinoma
- Olfactory Neuroblastoma
Not all midline tumours can be approached using the endonasal technique. A different minimally invasive procedure, like a standard craniotomy or a supraorbital eyebrow craniotomy, might be suggested for certain patients.
Potential Challenges and Considerations
- Despite being a major breakthrough, EETA requires a highly qualified surgical team. Important difficulties include:
- CSF leak risk, which calls for careful dural closure
- Possibility of incomplete tumour removal, especially in cases of invasive macroadenomas
- Expert rhinologists are required to handle the complex nasal structure.
In conclusion
In the treatment of pituitary adenoma, the endoscopic endonasal transsphenoidal technique represents a paradigm change. It provides a great substitute for traditional approaches due to its less invasive nature, enhanced visualisation, and quicker recovery. This method keeps developing as technology does, improving surgical accuracy and patient outcomes even further.
Source:
- https://www.yalemedicine.org/clinical-keywords/endonasal-transsphenoidal-approach#:~:text=Definition,the%20nose%20and%20sphenoid%20sinus.
- https://pubmed.ncbi.nlm.nih.gov/21181278/
- https://www.sciencedirect.com/science/article/pii/S2214751921000487
- https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2021.643550/full
- https://www.pacificneuroscienceinstitute.org/pituitary-disorders/treatment/endoscopic-endonasal-surgery/#:~:text=The%20endonasal%20route%20is%20the,chordomas%20and%20many%20midline%20menigiomas.
- https://www.mayoclinic.org/diseases-conditions/pituitary-tumors/symptoms-causes/syc-20350548
- https://www.cancer.gov/publications/dictionaries/cancer-terms/def/pituitary-tumor
- https://www.ninds.nih.gov/health-information/disorders/pituitary-tumors
You May Also Know Related to Gamma Knife
FAQ’s
How does Gamma Knife work?
Gamma Knife uses 192–201 precisely focused beams of gamma rays that converge at a single target point in the brain. This high dose of radiation damages the DNA of abnormal cells, stopping their growth or causing them to shrink, while minimizing exposure to nearby healthy tissue.
Is Gamma Knife a surgery?
No, Gamma Knife is not a traditional surgery. It is a non-invasive outpatient procedure performed without any incision, stitches, or general anesthesia in most cases.
What conditions can be treated with Gamma Knife?
Gamma Knife is commonly used for:
Brain tumors (benign and malignant)
Metastatic brain lesions
Arteriovenous malformations (AVMs)
Trigeminal neuralgia
Acoustic neuromas (vestibular schwannomas)
Pituitary tumors
Certain functional disorders (like tremors)
Is Gamma Knife painful?
The procedure is generally painless. Patients may feel mild pressure while the head frame (if used) is applied or may experience slight discomfort from anesthesia injections, but the treatment itself is not painful.
How long does the procedure take?
Depending on the condition and treatment plan, Gamma Knife may take 30 minutes to 3 hours. Most patients go home the same day.
What are the possible side effects?
Common side effects are usually mild and temporary, including:
Headache
Nausea
Fatigue
Mild scalp swelling or tenderness at the frame site
Rarely, some patients may experience delayed radiation effects such as brain swelling or radiation necrosis.
When can the patient return to normal activities after Gamma Knife?
Most patients can return to their normal routine within 24–48 hours after the procedure.
You may feel mild fatigue for a few days.
Follow-up imaging is usually required after 1 year.
How effective is Gamma Knife?
Gamma Knife has a high success rate and has been used worldwide for decades. Its effectiveness depends on the condition treated, size and location of the lesion, and overall patient health. In many cases, it offers results comparable to open surgery with fewer risks.
Can Gamma Knife be repeated if needed?
Yes, in some cases Gamma Knife treatment can be repeated if the disease recurs or if new lesions develop.
Is Gamma Knife safe?
Yes. Gamma Knife is considered one of the safest and most precise forms of radiosurgery, with millions of patients treated globally and extensive clinical data supporting its use.
Who is eligible for Gamma Knife treatment?
Eligibility depends on factors such as:
Size and location of the lesion
Overall health and age
Whether open surgery is too risky
A neurosurgeon and radiation oncologist will decide if Gamma Knife is the best option for you.
What happens before the procedure?
A detailed MRI or CT scan is performed to map the brain.
A lightweight head frame or mask is used for accuracy.
Your doctors plan the radiation dose and target areas using specialized software.
Will I need anesthesia?
Local anesthesia is given if a head frame is used.
General anesthesia is usually not required, except for children or patients unable to remain still.
What is the cost of Gamma Knife in India?
Costs vary depending on hospital, city, and condition treated. On average, Gamma Knife in India ranges from ₹1.5 lakh to ₹4.5 lakh. It is usually more affordable compared to treatment in Western countries. At AIIMS Delhi, it is much more affordable around ₹75,000 which makes it affordable for the patients in need.
Where can I get Gamma Knife treatment in Delhi?
AIIMS Delhi is one of the leading centres for Gamma Knife in India.
AIIMS uses the latest Gamma Knife Perfexion system.
It has successfully treated thousands of patients for brain tumors, blood vessel problems, and even eye cancers.
The treatment is done by expert neurosurgeons such as Dr. Deepak Agrawal and team.
Clinic timings for Gamma Knife OPD at AIIMS Delhi: Monday & Friday, 8:00 AM – 9:00 AM.
Cost is around ₹75,000 and is subsidized compared to private hospitals.
What is the complete process of the Gamma Knife?
The whole procedure is usually done in one day:
- Consultation & Planning – Doctors review your scans and decide the treatment.
- Head Frame/Mask – A lightweight frame or mask is placed to keep your head still.
- Imaging – MRI/CT scans are done to locate the exact target.
- Treatment Planning – Specialists plan the dose and direction of radiation.
- Gamma Knife Treatment – You lie on the machine; painless radiation beams treat the target (30 mins–3 hrs).
- Recovery & Discharge – The frame is removed, and most patients go home the same day.
- Follow-up – MRI after a few months to check results.
What formalities do I have to complete prior to getting the date of GK?
Before you get a treatment date, you need to complete a few steps:
- OPD Registration – Visit the Neurosurgery OPD (Gamma Knife clinic at AIIMS, Mon & Fri 8–9 AM) and register.
- Consultation with Doctor – Meet the neurosurgeon who will check your reports, MRI/CT scans, and medical history.
- Investigations – Sometimes fresh MRI/CT or blood tests are needed for treatment planning.
- Medical Fitness – Basic checks like blood pressure, sugar, heart condition, etc.
Financial/Insurance Approval –
- If using Ayushman Bharat or government schemes, you need approval papers.
- If self-paying, you will be given the estimated cost (~₹75,000 at AIIMS).
- Consent & Admission Slip – Once doctors confirm you are fit and formalities are done, you sign the consent form.
- Treatment Date Allotment – A date is given for your Gamma Knife procedure.
What formalities do I have to complete after getting the date of GK?
Once you receive your Gamma Knife date, you’ll need to do a few simple things before the procedure:
- Admission Process – Report to AIIMS on the morning of your procedure and complete admission at the Neurosurgery ward/Daycare.
- Paperwork – Carry your OPD slip, MRI/CT films, blood test reports, admission slip, and ID proof. If you are covered under Ayushman Bharat/insurance, keep those approval papers ready.
- Consent Forms – You (or a family member) will sign consent for the procedure and anesthesia.
- Medical Check-up – Doctors will check your BP, sugar, heart rate, and do a quick physical exam.
- Fasting – Usually, you will be asked to not eat or drink for 6 hours before the procedure.
- Pre-Procedure Prep – An IV line may be put, and medicines (sedation/antibiotics if needed) are given.
- Treatment – You are then taken to the Gamma Knife room for frame/mask placement, imaging, and treatment.
After the procedure, you’ll be observed for a few hours and most patients are discharged the same day or next morning.
What investigations to be done?
Urea & creatinine
Should I come fasting?
No, You can have light breakfast.
In case of HT/DM should take my medicines?
Yes, you can take the medicine and then come for the treatment.